Aetna Stelara Prior Authorization Form - Web please read the accompanying important brief summary for stelara® and discuss any questions you have with your doctor. Aeta specialty precertification forms abatacept. Web program prior authorization/medical necessity medication *stelara™ (ustekinumab) *this program applies to. Web specialty medication precertification request please indicate: Web an aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not listed as eligible. Web stelara®(ustekinumab) specialty medication precertification request. Web aetna pharmacy management administers, but does not offer, insure or otherwise underwrite the. Web what is prior authorization? Web tofacitinib (xeljanz tm) medication precertification request form (pdf, 375 kb) trastuzumab (herceptin), ado. The services that need prior authorization.
Aetna GR690251 CO 2016 Fill and Sign Printable Template Online US
Web please read the accompanying important brief summary for stelara® and discuss any questions you have with your doctor. Web apply a check mark to indicate the answer where needed. Web for part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. Web the basics of prior authorization. Web.
Gallery of Aetna Better Health Prior Auth form Inspirational Aarp
Web what is prior authorization? Web the basics of prior authorization. Web program prior authorization/medical necessity medication *stelara™ (ustekinumab) *this program applies to. Precertification of intravenous ustekinumab (stelara iv) is required of all aetna participating. Double check all the fillable fields to ensure full accuracy.
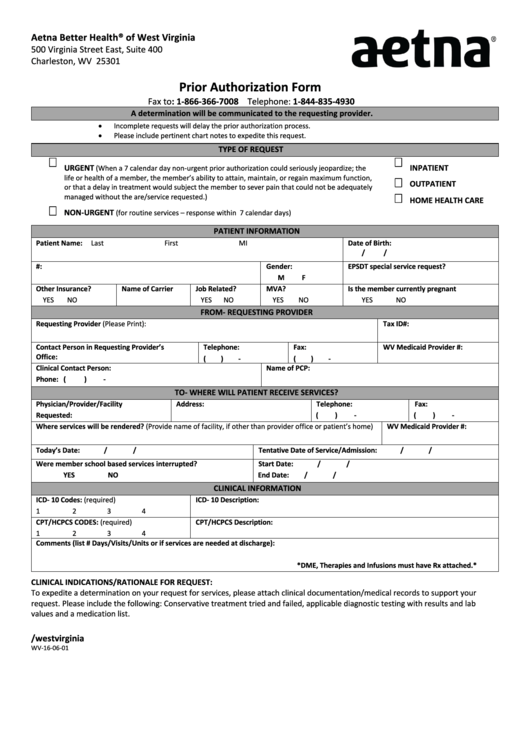
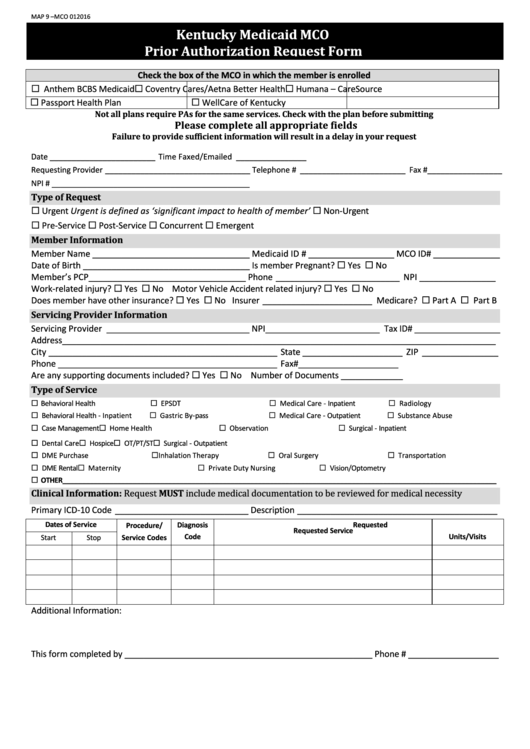
From Wv160601 Aetna Prior Authorization Form printable pdf download
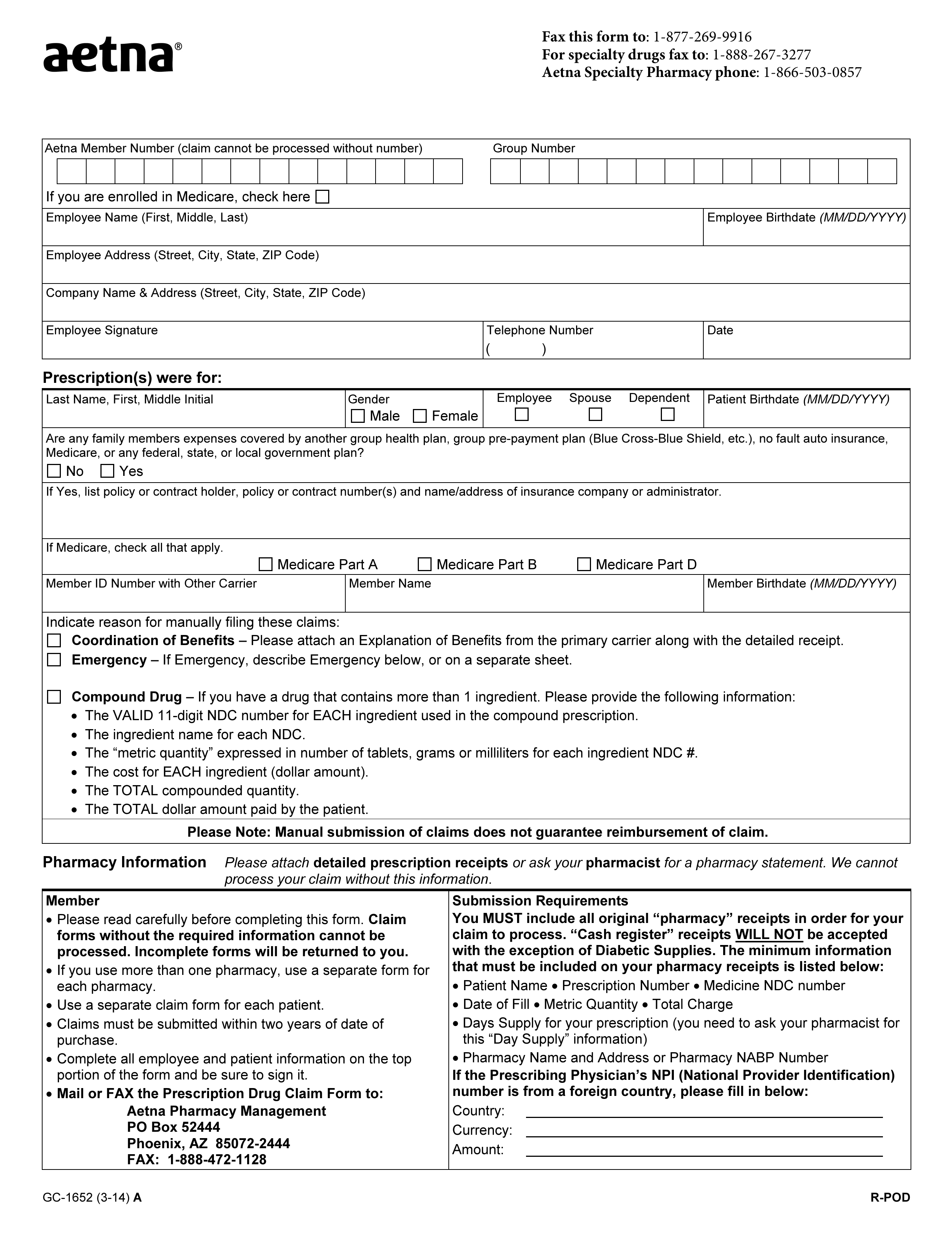
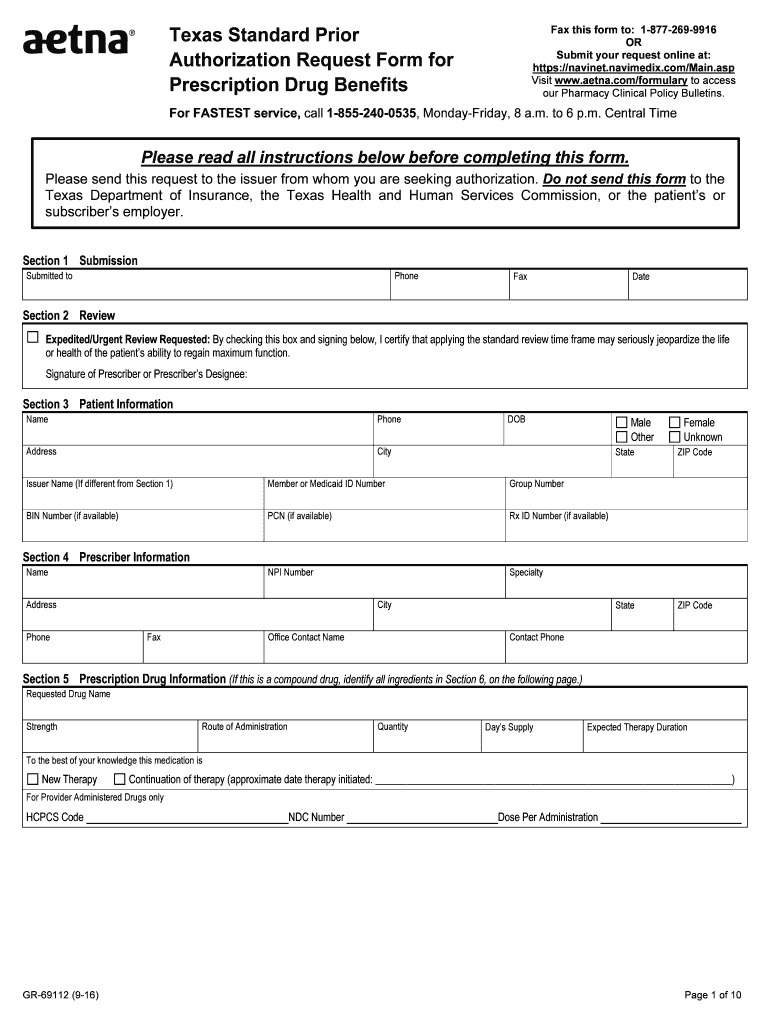
Web prior authorization you or your doctor needs approval from us before we cover the drug. Web an aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not listed as eligible. Web for part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy..
Walgreens Specialty Pharmacy Launches HIV Focused Web Site PDF
Web specialty medication precertification request please indicate: Web apply a check mark to indicate the answer where needed. Web discover the documents and forms you required to request specialty drug. Web an aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not listed as eligible. Some procedures, tests and prescriptions need prior approval to.
Aetna Prior Authorization Form Medical Record Health Sciences
Web apply a check mark to indicate the answer where needed. Web specialty medication precertification request please indicate: The services that need prior authorization. Specialty medication precertification request page. Web prior authorization you or your doctor needs approval from us before we cover the drug.
Where Do You Sign Up For Medicare September 2017
Web aetna pharmacy management administers, but does not offer, insure or otherwise underwrite the. Stelara subcutaneous taltz xeljanz xeljanz. Some procedures, tests and prescriptions need prior approval to be sure they’re right for. Web medicare form stelara®(ustekinumab) specialty medication precertification request for medicare advantage part b:. Check out this section to learn what it is and why it’s important.
We do not even must be two people with gender, in all honesty aikosia
Web stelara®(ustekinumab) specialty medication precertification request. Web for part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. Web a way to find out if stelara® is covered by the patient's insurance plan, including requirements for coverage or. Web home stelara ® insurance coverage prior authorizations exceptions appeals in.
Aetna Specialty Pharmacy Prior Authorization Form PharmacyWalls
Web program prior authorization/medical necessity medication *stelara™ (ustekinumab) *this program applies to. Double check all the fillable fields to ensure full accuracy. Web medicare form stelara®(ustekinumab) specialty medication precertification request for medicare advantage part b:. The services that need prior authorization. Web home stelara ® insurance coverage prior authorizations exceptions appeals in certain states, a standardized.
Aetna Standard Prior Form Fill Out and Sign Printable PDF Template
Web stelara® (ustekinumab) specialty medication precertification request page 1 of 3 (all fields. Web please read the accompanying important brief summary for stelara® and discuss any questions you have with your doctor. Web medicare form stelara®(ustekinumab) specialty medication precertification request for medicare advantage part b:. Web an aetna prior authorization form is designated for medical offices when a particular patient’s.
Gallery of Aetna Better Health Prior Auth form Lovely Future Scripts
During the prior authorization process, it’s reviewed against nationally recognized criteria, the highest. Check out this section to learn what it is and why it’s important. Web stelara® (ustekinumab) specialty medication precertification request page 1 of 3 (all fields. Web what is prior authorization? Web a way to find out if stelara® is covered by the patient's insurance plan, including.
Aeta specialty precertification forms abatacept. Web please read the accompanying important brief summary for stelara® and discuss any questions you have with your doctor. Web aetna pharmacy management administers, but does not offer, insure or otherwise underwrite the. Web medicare form stelara®(ustekinumab) specialty medication precertification request for medicare advantage part b:. Some procedures, tests and prescriptions need prior approval to be sure they’re right for. Specialty medication precertification request page. Web program prior authorization/medical necessity medication *stelara™ (ustekinumab) *this program applies to. Web stelara® (ustekinumab) specialty medication precertification request page 1 of 3 (all fields. Web home stelara ® insurance coverage prior authorizations exceptions appeals in certain states, a standardized. Web an aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not listed as eligible. Web prior authorization you or your doctor needs approval from us before we cover the drug. During the prior authorization process, it’s reviewed against nationally recognized criteria, the highest. The services that need prior authorization. Web stelara®(ustekinumab) specialty medication precertification request. Web for part d prior authorization forms, see the medicare precertification section or the medicare medical specialty drug and part b step therapy. Web apply a check mark to indicate the answer where needed. Web discover the documents and forms you required to request specialty drug. Precertification of intravenous ustekinumab (stelara iv) is required of all aetna participating. Double check all the fillable fields to ensure full accuracy. Check out this section to learn what it is and why it’s important.
Web Medicare Form Stelara®(Ustekinumab) Specialty Medication Precertification Request For Medicare Advantage Part B:.
Double check all the fillable fields to ensure full accuracy. Aeta specialty precertification forms abatacept. Web stelara®(ustekinumab) specialty medication precertification request. Web discover the documents and forms you required to request specialty drug.
Stelara Subcutaneous Taltz Xeljanz Xeljanz.
Web a way to find out if stelara® is covered by the patient's insurance plan, including requirements for coverage or. Web program prior authorization/medical necessity medication *stelara™ (ustekinumab) *this program applies to. Web the basics of prior authorization. Web an aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not listed as eligible.
Web Please Read The Accompanying Important Brief Summary For Stelara® And Discuss Any Questions You Have With Your Doctor.
Web stelara® (ustekinumab) specialty medication precertification request page 1 of 3 (all fields. Check out this section to learn what it is and why it’s important. Web home stelara ® insurance coverage prior authorizations exceptions appeals in certain states, a standardized. Web what is prior authorization?
Web For Part D Prior Authorization Forms, See The Medicare Precertification Section Or The Medicare Medical Specialty Drug And Part B Step Therapy.
Specialty medication precertification request page. During the prior authorization process, it’s reviewed against nationally recognized criteria, the highest. Precertification of intravenous ustekinumab (stelara iv) is required of all aetna participating. Web aetna pharmacy management administers, but does not offer, insure or otherwise underwrite the.