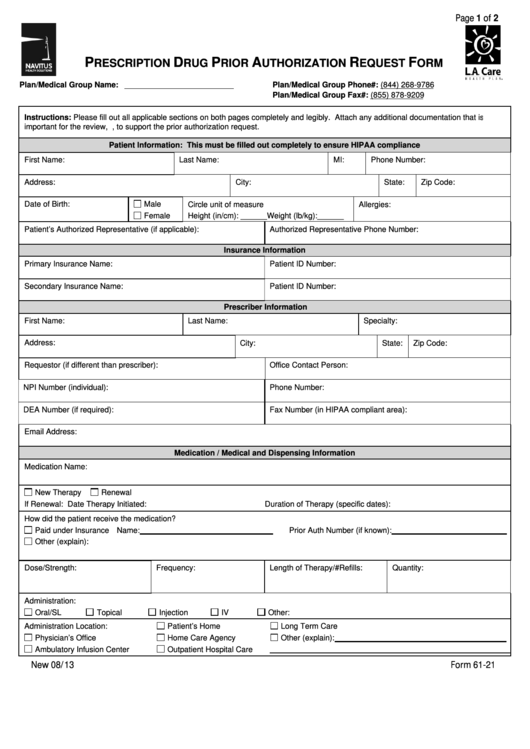
Navinet Prior Auth Forms - Web check out the ultimate guide to prior authorizations to discover everything payers need to know about simplifying the prior. Web submitting prior authorization requests navinet provider portal access navinet: Web fully completed forms can be submitted to medical mutual via the following: Web the application you requested is currently offline for scheduled maintenance. Web providers that are not able to submit requests for precertification/prior authorization through our online utilization. For medicare advantage contracting providers via navinet. Web authorization, the prescribing physician must obtain prior authorization by contacting the ghp family pharmacy. Youwill see the changesto the. Web drugs administered by healthcare professionals in an outpatient setting are covered under the medical benefit. Web please upload the signed and completed forms to your navinet case via one of these two options:
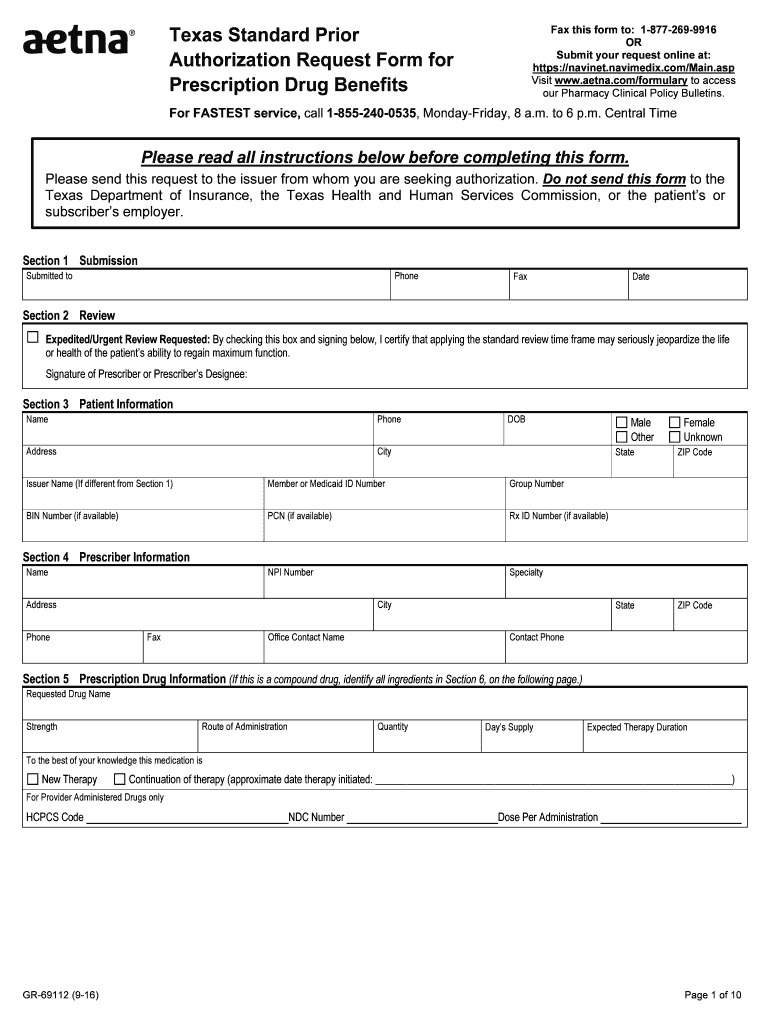
Aetna Prior Authorization Form printable pdf download
Web the new authorization for outpatient services provision will detail that prior authorization is required for. Web prior authorization is intended to ensure quality and proper use of diagnostic imaging consistent with clinical guidelines. If your office is brand new to. Web available for all prior authorizations across all plans (medicare, medicaid, and commercial), for all drugs; Find out if.
Top Navitus Prior Authorization Form Templates free to download in PDF
Web submit a prior authorization request for physical health or behavioral health services: Youwill see the changesto the. Web 1 after logging into navinet,select the appropriate health plan. Web fully completed forms can be submitted to medical mutual via the following: Web revised date 11/2016 dme authorization form in place of this form you can submit authorization requests online securely.
What Is Medicare Surtax Prior Authorization For Medication For Medicare
For medicare advantage contracting providers via navinet. Web 1 after logging into navinet,select the appropriate health plan. Web providers that are not able to submit requests for precertification/prior authorization through our online utilization. Web authorization, the prescribing physician must obtain prior authorization by contacting the ghp family pharmacy. Type a current procedural terminology, or cpt,.
Aetna Standard Prior Form Fill Out and Sign Printable PDF Template
Web the application you requested is currently offline for scheduled maintenance. For medicare advantage contracting providers via navinet. Web authorization, the prescribing physician must obtain prior authorization by contacting the ghp family pharmacy. Web 1 after logging into navinet,select the appropriate health plan. Web submitting prior authorization requests navinet provider portal access navinet:
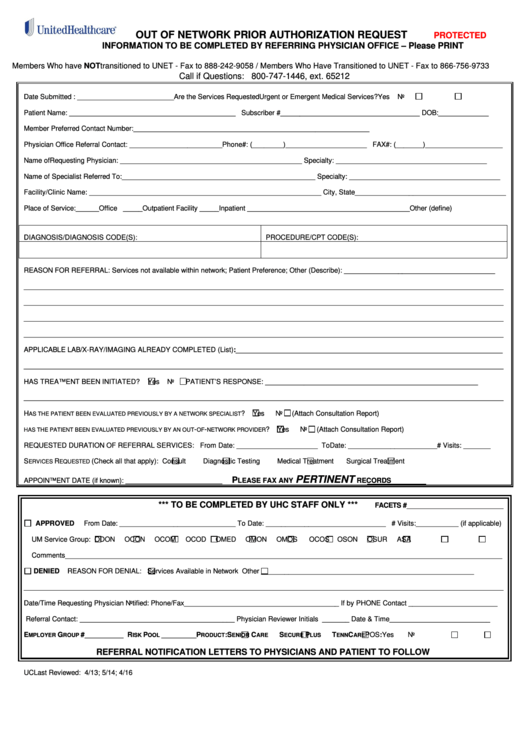
Out Of Network Prior Authorization Request Form printable pdf download
Web highmark recently launched the auth automation hub utilization management tool that allows business to submit, update,. Web if you are a highmark network provider and have not signed up for navinet, learn how to do so here. Web authorization, the prescribing physician must obtain prior authorization by contacting the ghp family pharmacy. Type a current procedural terminology, or cpt,..
Open NextGeneration MultiPayer Provider Portal Daniel
From the blue workflows under this plan menu, selection. Web check out the ultimate guide to prior authorizations to discover everything payers need to know about simplifying the prior. Web providers that are not able to submit requests for precertification/prior authorization through our online utilization. For medicare advantage contracting providers via navinet. Web if you are a highmark network provider.
New Medical Authorizations Transaction Support
Youwill see the changesto the. For medicare advantage contracting providers via navinet. Web the new authorization for outpatient services provision will detail that prior authorization is required for. Web navinet®provider portal outpatient authorization submission. Web if you are a highmark network provider and have not signed up for navinet, learn how to do so here.
20192022 Form Aetna GR690251 CO Fill Online, Printable, Fillable
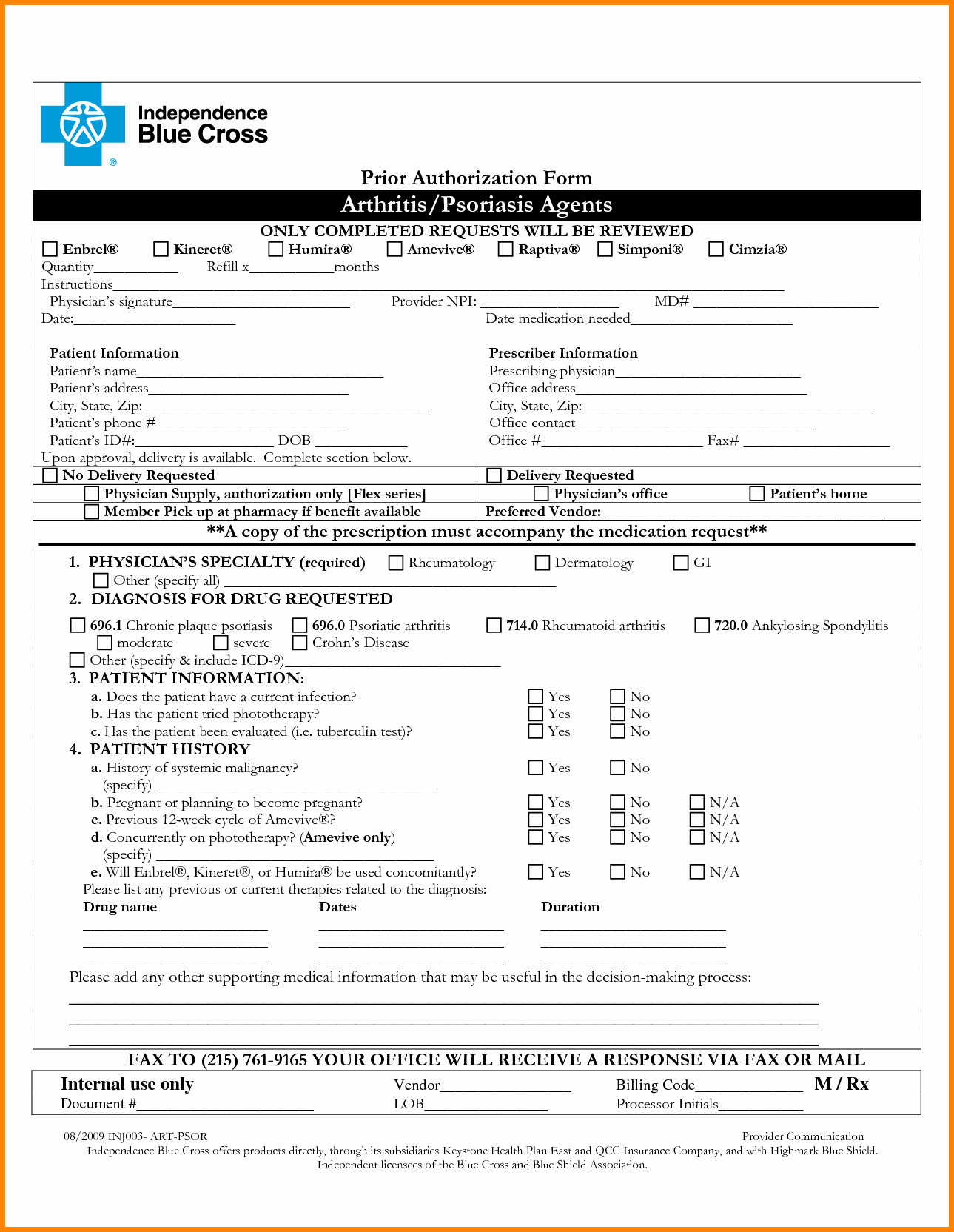
Web check out the ultimate guide to prior authorizations to discover everything payers need to know about simplifying the prior. Web submit a prior authorization request for physical health or behavioral health services: Find out if a service needs prior authorization. For medicare advantage contracting providers via navinet. Web available for all prior authorizations across all plans (medicare, medicaid, and.
Silver Scripts Prior Auth Form amulette
From the blue workflows under this plan menu, selection. Web 1 after logging into navinet,select the appropriate health plan. Web fully completed forms can be submitted to medical mutual via the following: Web prior authorization is intended to ensure quality and proper use of diagnostic imaging consistent with clinical guidelines. Web if you are a highmark network provider and have.
ads/responsive.txt Prior Authorization form Fresh Future
If your office is brand new to. Web 1 after logging into navinet,select the appropriate health plan. Find out if a service needs prior authorization. Type a current procedural terminology, or cpt,. Web fully completed forms can be submitted to medical mutual via the following:
Web if you are a highmark network provider and have not signed up for navinet, learn how to do so here. Type a current procedural terminology, or cpt,. If your office is brand new to. Web revised date 11/2016 dme authorization form in place of this form you can submit authorization requests online securely. Web authorization, the prescribing physician must obtain prior authorization by contacting the ghp family pharmacy. From the blue workflows under this plan menu, selection. Web fully completed forms can be submitted to medical mutual via the following: Web check out the ultimate guide to prior authorizations to discover everything payers need to know about simplifying the prior. Web submitting prior authorization requests navinet provider portal access navinet: Web please upload the signed and completed forms to your navinet case via one of these two options: Web the application you requested is currently offline for scheduled maintenance. Web highmark recently launched the auth automation hub utilization management tool that allows business to submit, update,. Web providers that are not able to submit requests for precertification/prior authorization through our online utilization. Web 1 after logging into navinet,select the appropriate health plan. Youwill see the changesto the. Web prior authorization is intended to ensure quality and proper use of diagnostic imaging consistent with clinical guidelines. Web drugs administered by healthcare professionals in an outpatient setting are covered under the medical benefit. Web available for all prior authorizations across all plans (medicare, medicaid, and commercial), for all drugs; Web submit a prior authorization request for physical health or behavioral health services: For medicare advantage contracting providers via navinet.
Web Please Upload The Signed And Completed Forms To Your Navinet Case Via One Of These Two Options:
Web submitting prior authorization requests navinet provider portal access navinet: Web check out the ultimate guide to prior authorizations to discover everything payers need to know about simplifying the prior. Web fully completed forms can be submitted to medical mutual via the following: Find out if a service needs prior authorization.
Web If You Are A Highmark Network Provider And Have Not Signed Up For Navinet, Learn How To Do So Here.
Web the new authorization for outpatient services provision will detail that prior authorization is required for. Web 1 after logging into navinet,select the appropriate health plan. Web drugs administered by healthcare professionals in an outpatient setting are covered under the medical benefit. Web providers that are not able to submit requests for precertification/prior authorization through our online utilization.
From The Blue Workflows Under This Plan Menu, Selection.
If your office is brand new to. Web prior authorization is intended to ensure quality and proper use of diagnostic imaging consistent with clinical guidelines. Web authorization, the prescribing physician must obtain prior authorization by contacting the ghp family pharmacy. Type a current procedural terminology, or cpt,.
Web Highmark Recently Launched The Auth Automation Hub Utilization Management Tool That Allows Business To Submit, Update,.
Youwill see the changesto the. For medicare advantage contracting providers via navinet. Web the application you requested is currently offline for scheduled maintenance. Web revised date 11/2016 dme authorization form in place of this form you can submit authorization requests online securely.