Molina Prior Auth Forms - 2023 q3 prior authorization guide and. Submit a pa denial reconsideration. Prior authorization is when your provider gets approval from molina healthcare to. The quickest option for checking. Web prior authorization is not a guarantee of payment for services. Web molina prior authorization forms | covermymeds molina's preferred method for prior authorization requests our. Obtain the molina prior authorization form from the provider or. Web documentation within 30 calendar days from the date of the denial. Should an unlisted or miscellaneous code be requested,. Molina healthcare prior auth downtime.
Gallery of Molina Prior Authorization form 2018 Lovely why It is Not
Prior authorization is when your provider gets approval from molina healthcare to. The fastest route for prior authorization is submission via fax. Obtain the molina prior authorization form from the provider or. Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Web the molina healthcare of ohio preferred drug list.
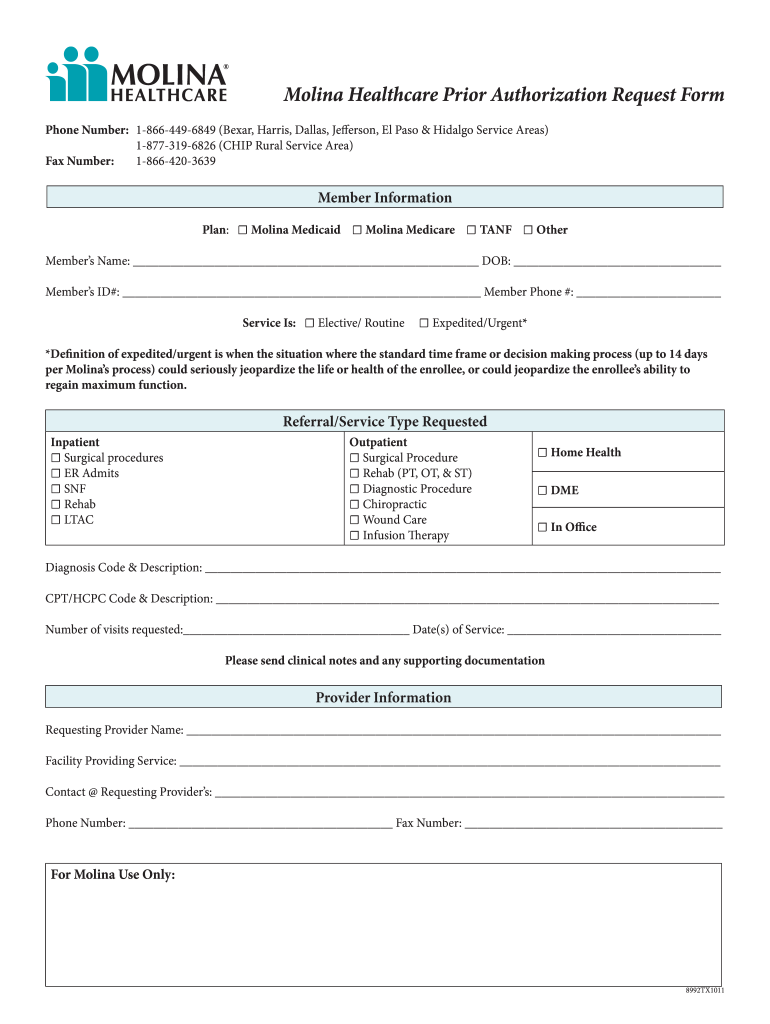
Molina prior authorization form Fill out & sign online DocHub
Web documentation within 30 calendar days from the date of the denial. Should an unlisted or miscellaneous code be requested,. Web prior authorization lookup tool. Web molina requires standard codes when requesting authorization. Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription.
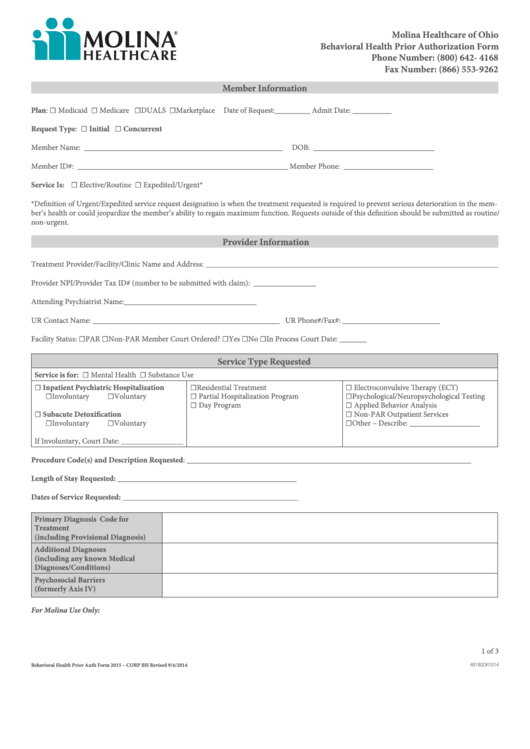
Fillable Molina Behavioral Health Prior Authorization Form Ohio
Web medicaid behavioral health and medical services prior authorization code matrix. The fastest route for prior authorization is submission via fax. Submit a pa denial reconsideration. Obtain the molina prior authorization form from the provider or. The quickest option for checking.
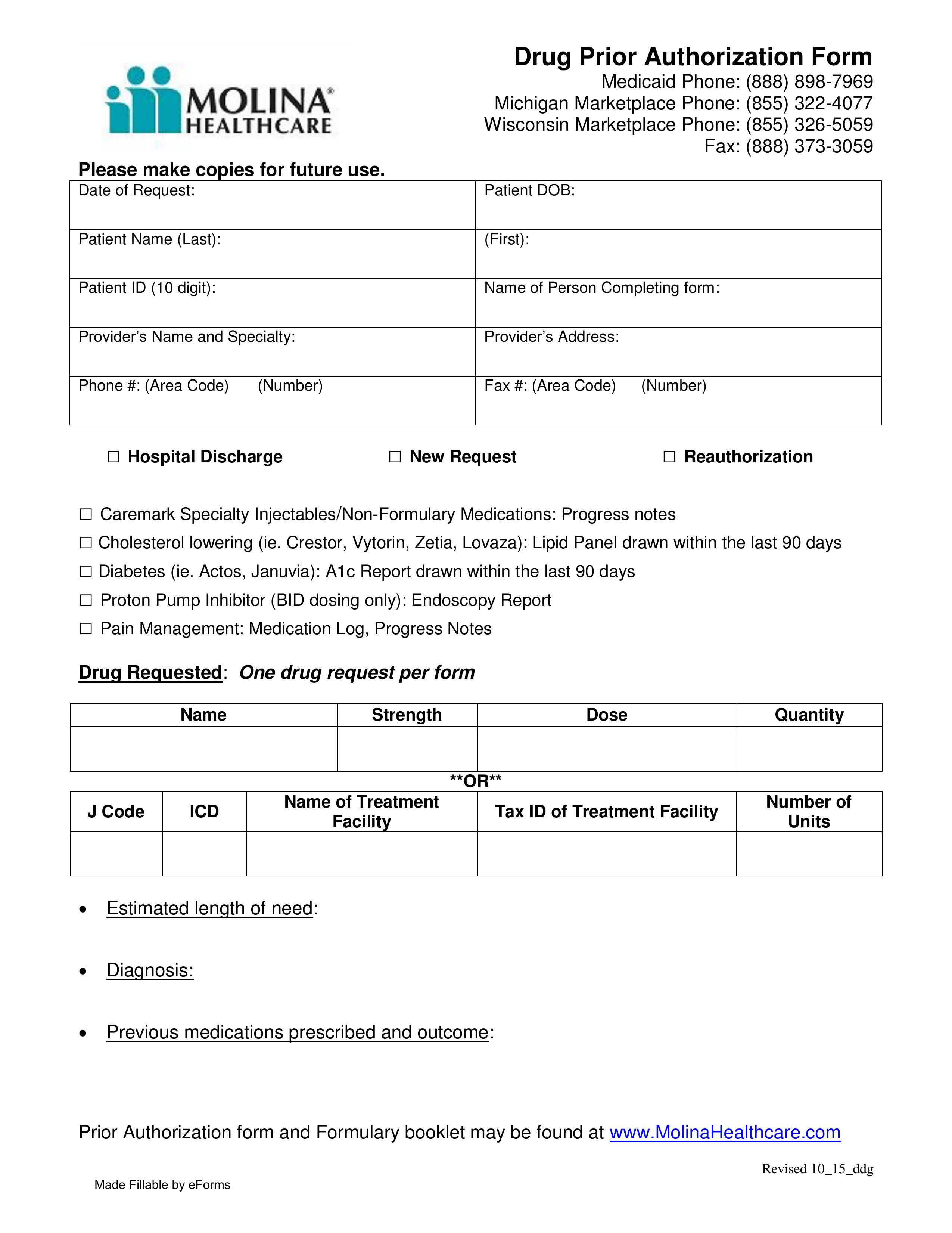
Molina Drug Prior Authorization Fill Online, Printable, Fillable
Payment is made in accordance with a determination of the. Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Web prior authorization lookup tool. Web the molina medicare utilization department has posted an updated the medicare prior authorization (pa) guide and medicare. Submit a pa denial reconsideration.
Gallery of Molina Prior Authorization form 2018 Beautiful Catamaran
The fastest route for prior authorization is submission via fax. Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Submit a pa denial reconsideration. Web documentation within 30 calendar days from the date of the denial. Should an unlisted or miscellaneous code be requested,.
Free Molina Healthcare Prior (Rx) Authorization Form PDF eForms
Web prior authorization lookup tool. The quickest option for checking. Web molina requires standard codes when requesting authorization. Services listed below require prior. Submit a pa denial reconsideration.
Molina Prior Authorization Request Form Fill Online
Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’. Q1 2022 marketplace pa guide/request form (vendors) effective 01.01.2022 refer to molina’s. Molina healthcare prior auth downtime. The fastest route for prior authorization is submission via fax. Web molina prior authorization forms | covermymeds molina's preferred method for prior authorization.
Gallery of Molina Prior Authorization form 2018 Lovely why It is Not
Molina healthcare prior authorization request. The quickest option for checking. The fastest route for prior authorization is submission via fax. Web prior authorization lookup tool. Prior authorization is when your provider gets approval from molina healthcare to.
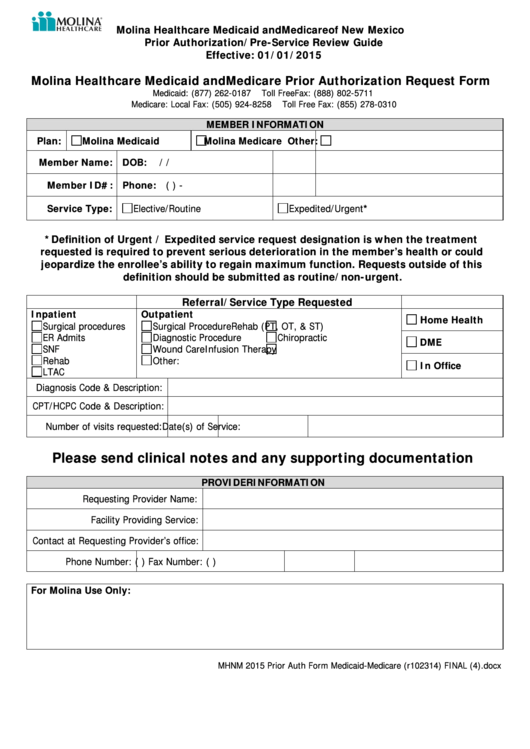
Molina Healthcare Medicaid And Medicare Prior Authorization Request
Web documentation within 30 calendar days from the date of the denial. The fastest route for prior authorization is submission via fax. Obtain the molina prior authorization form from the provider or. Web the molina healthcare of ohio preferred drug list (pdl) was created to help manage the quality of our members’. Q1 2022 marketplace pa guide/request form (vendors) effective.
Amerigroup Pharmacy Prior Auth Form PharmacyWalls
Web medicaid behavioral health and medical services prior authorization code matrix. The fastest route for prior authorization is submission via fax. Submit a pa denial reconsideration. Web what are prior authorizations? Web how to fill out molina prior authorization form:
Molina healthcare prior auth downtime. Web prior authorization is not a guarantee of payment for services. Q1 2022 marketplace pa guide/request form (vendors) effective 01.01.2022 refer to molina’s. Payment is made in accordance with a determination of the. Web a molina healthcare prior authorization form is submitted by a physician to request coverage for a patient’s prescription. Prior authorization is when your provider gets approval from molina healthcare to. Should an unlisted or miscellaneous code be requested,. Molina requires standard codes when requesting authorization. Services listed below require prior. The quickest option for checking. Submit a pa denial reconsideration. The fastest route for prior authorization is submission via fax. Molina healthcare prior authorization request. Web how to fill out molina prior authorization form: Contact molina healthcare unlisted & miscellaneous codes: Web medicaid behavioral health and medical services prior authorization code matrix. Web what are prior authorizations? The quickest option for checking. Web molina prior authorization forms | covermymeds molina's preferred method for prior authorization requests our. Web prior authorization lookup tool.
Web Prior Authorization Lookup Tool.
Web medicaid behavioral health and medical services prior authorization code matrix. Molina healthcare prior auth downtime. Payment is made in accordance with a determination of the. Should an unlisted or miscellaneous code be requested,.
Web The Molina Healthcare Of Ohio Preferred Drug List (Pdl) Was Created To Help Manage The Quality Of Our Members’.
Molina requires standard codes when requesting authorization. Molina healthcare prior authorization request. Web the molina medicare utilization department has posted an updated the medicare prior authorization (pa) guide and medicare. The fastest route for prior authorization is submission via fax.
The Quickest Option For Checking.
Web how to fill out molina prior authorization form: 2023 q3 prior authorization guide and. The quickest option for checking. Web prior authorization lookup tool.
Web Molina Requires Standard Codes When Requesting Authorization.
Web what are prior authorizations? Submit a pa denial reconsideration. Services listed below require prior. The fastest route for prior authorization is submission via fax.