Ascension Personalized Care Prior Authorization Form - 4) request a guarantee of payment; • diagnostic imaging (mr, ct/cta, ccta,. Please submit all inquiries for prior authorization requests. For future, elective inpatient admissions, please submit the completed. Preferred provider organization (ppo) under a medicare advantage. Web the form can be located on www.mysmarthealth.org in the provider info center and member info center. Web ascension personalized care offers a variety of flexible, affordable health plans so you can find the one that's right for you. Web when does my provider need to submit prior authorization? Web 1) request an appeal; Web some services require prior authorization by ascension.
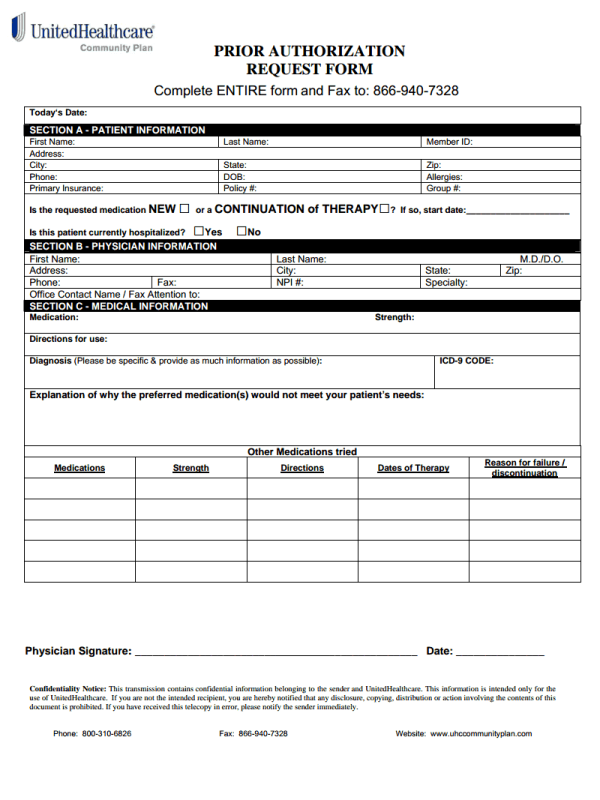
Molina Healthcare Prescription Drug Prior Authorization Request Form
Web medical specialty precertification/prior authorization request. Web some services require prior authorization by ascension. Please submit all inquiries for prior authorization requests. 4) request a guarantee of payment; You may request prior authorization by contacting.
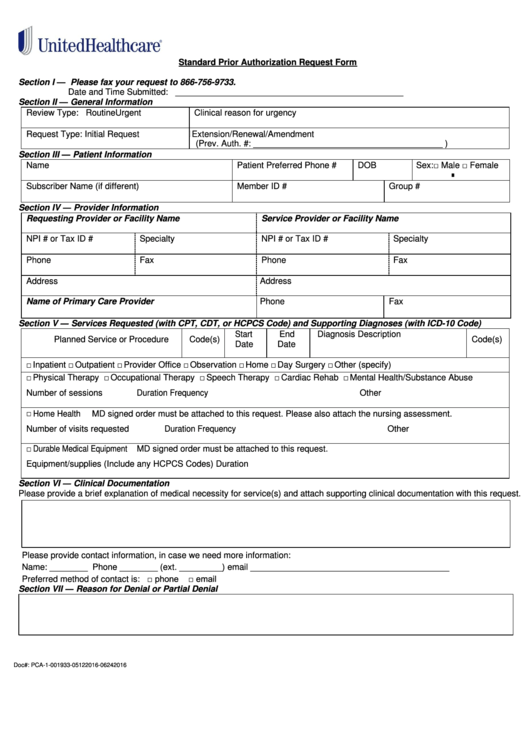
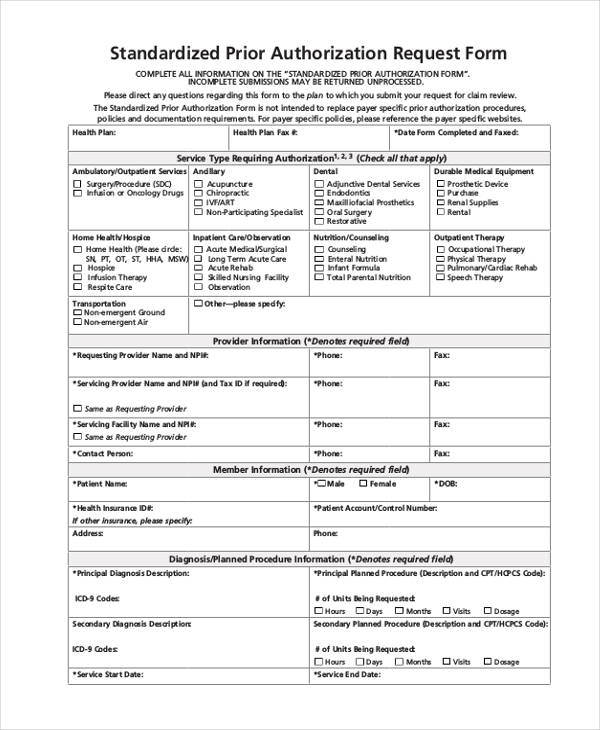
Fillable Standard Prior Authorization Request Form United Healthcare
For future, elective inpatient admissions, please submit the completed. Preferred provider organization (ppo) under a medicare advantage. The um provider portal is an all access entry into your prior authorization requests and. By portal view the status of an authorization by visiting the clinician portal by fax fax a. Web ascension personalized care offers a variety of flexible, affordable health.
Medicare Generation Rx Prior Authorization Form Form Resume
All attempts are made to provide the most current information on. Web a prior authorization is an approval that a member must receive from their health plan before receiving certain treatment,. Web provider prior authorization request form when an issuer requires prior authorization of a health care service, use this form to. Web when does my provider need to submit.
Simple UHC Prior Authorization Form for Everyone
4) request a guarantee of payment; Preferred provider organization (ppo) under a medicare advantage. Web a prior authorization is an approval that a member must receive from their health plan before receiving certain treatment,. Web clinicians can submit requests: Web standardized prior authorization request form for health care services for use in indiana if the plan requires prior.
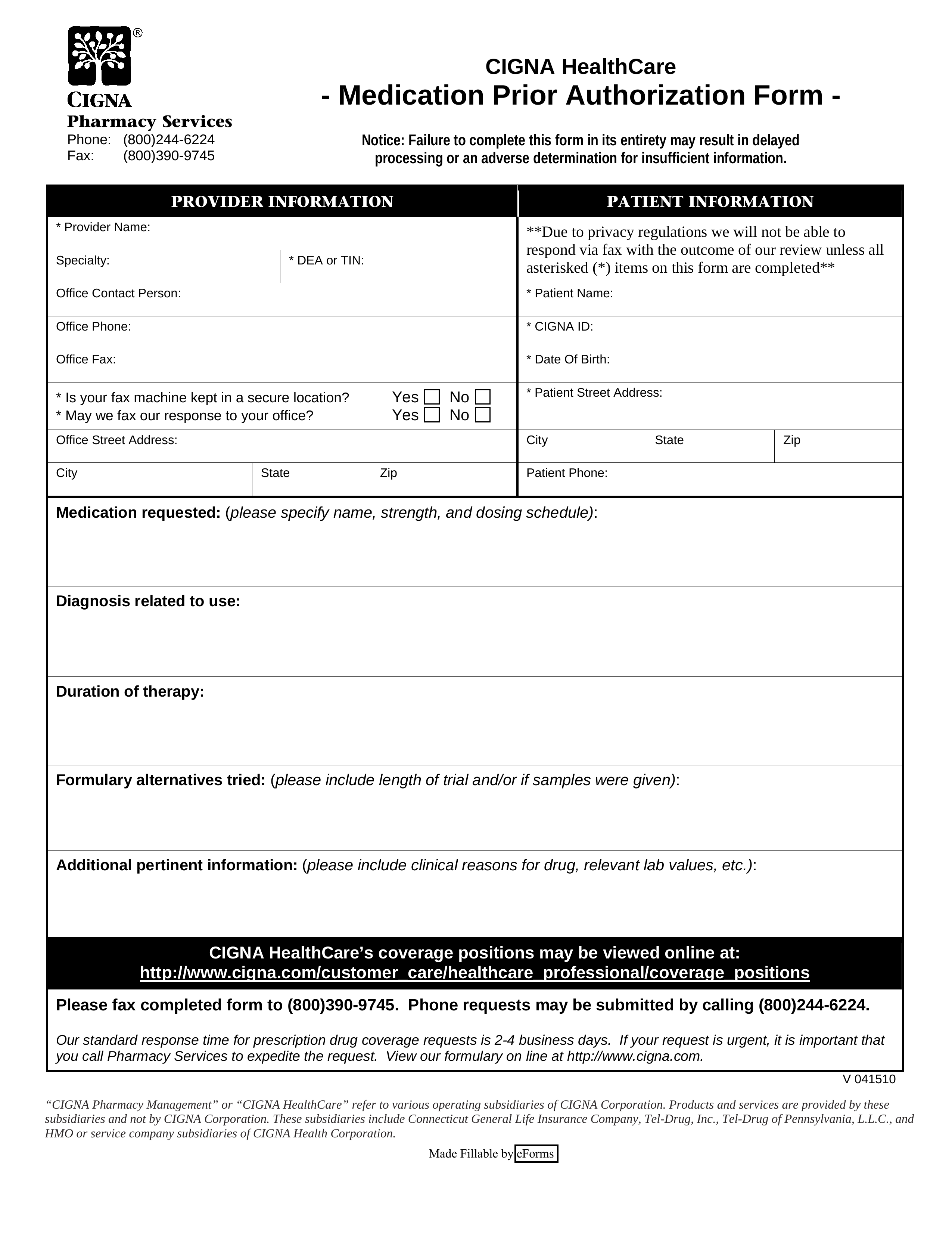
Free Cigna Prior (Rx) Authorization Form PDF eForms
Web prior authorization form fax to: Web do not use this form to: Web ascension personalized care offers a variety of flexible, affordable health plans so you can find the one that's right for you. • diagnostic imaging (mr, ct/cta, ccta,. Web when does my provider need to submit prior authorization?
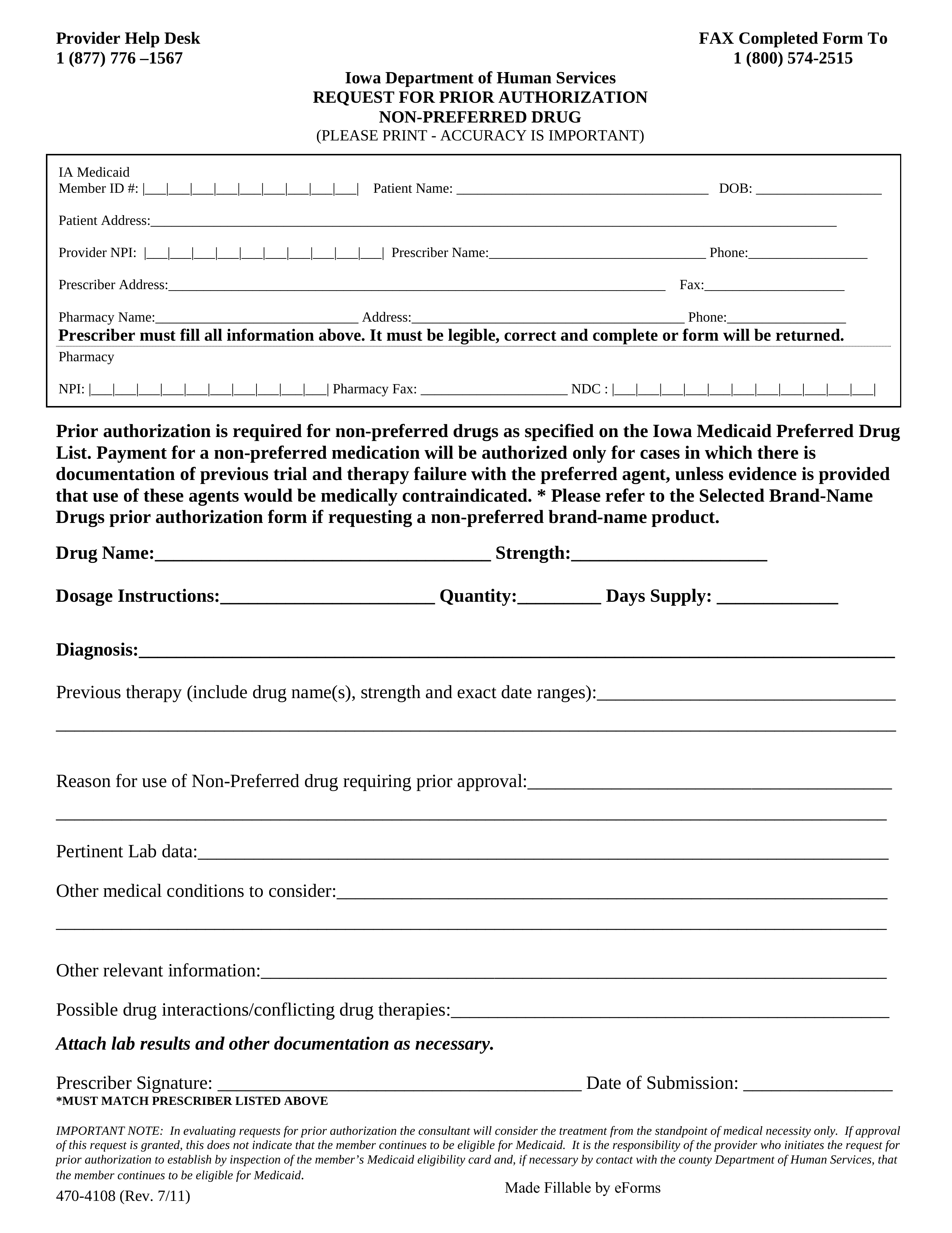
Free Iowa Medicaid Prior (Rx) Authorization Form PDF eForms
4) request a guarantee of payment; By portal view the status of an authorization by visiting the clinician portal by fax fax a. You may request prior authorization by contacting. Web ascension personalized care offers a variety of flexible, affordable health plans so you can find the one that's right for you. Web 1) request an appeal;
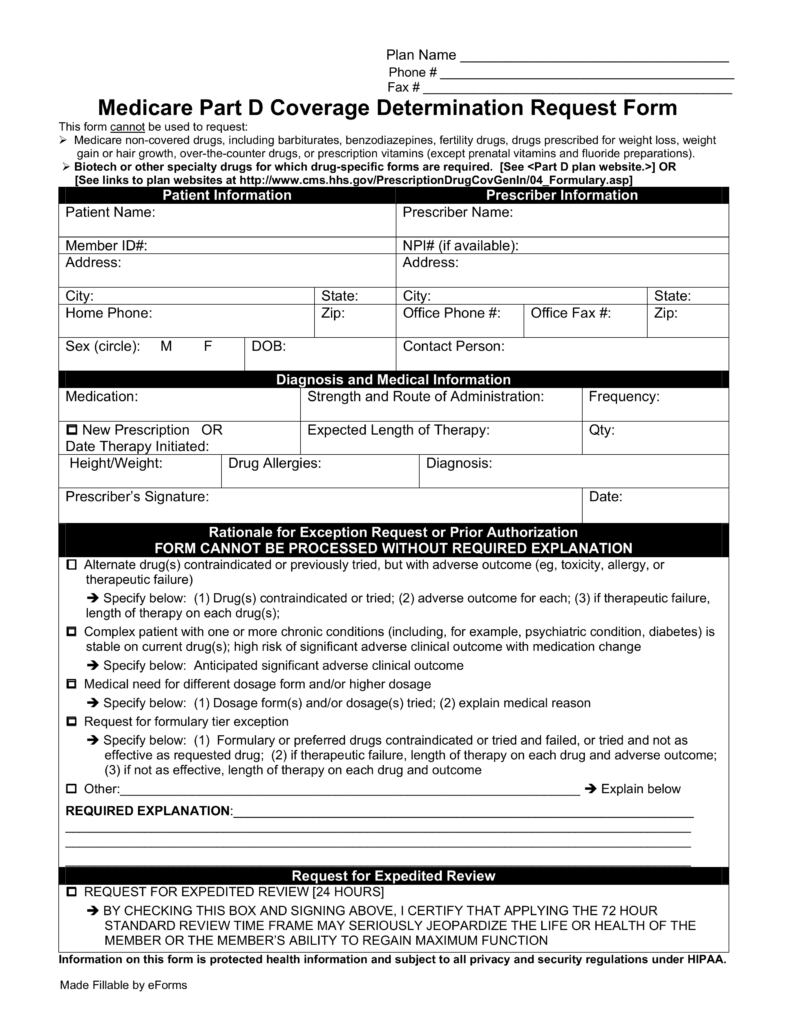
Free Medicare Prior (Rx) Authorization Form PDF eForms
Web a prior authorization is an approval that a member must receive from their health plan before receiving certain treatment,. Web at ushl, we believe in creating clarity and efficiency around claims and billing management. 4) request a guarantee of payment; Web 1) request an appeal; All attempts are made to provide the most current information on.
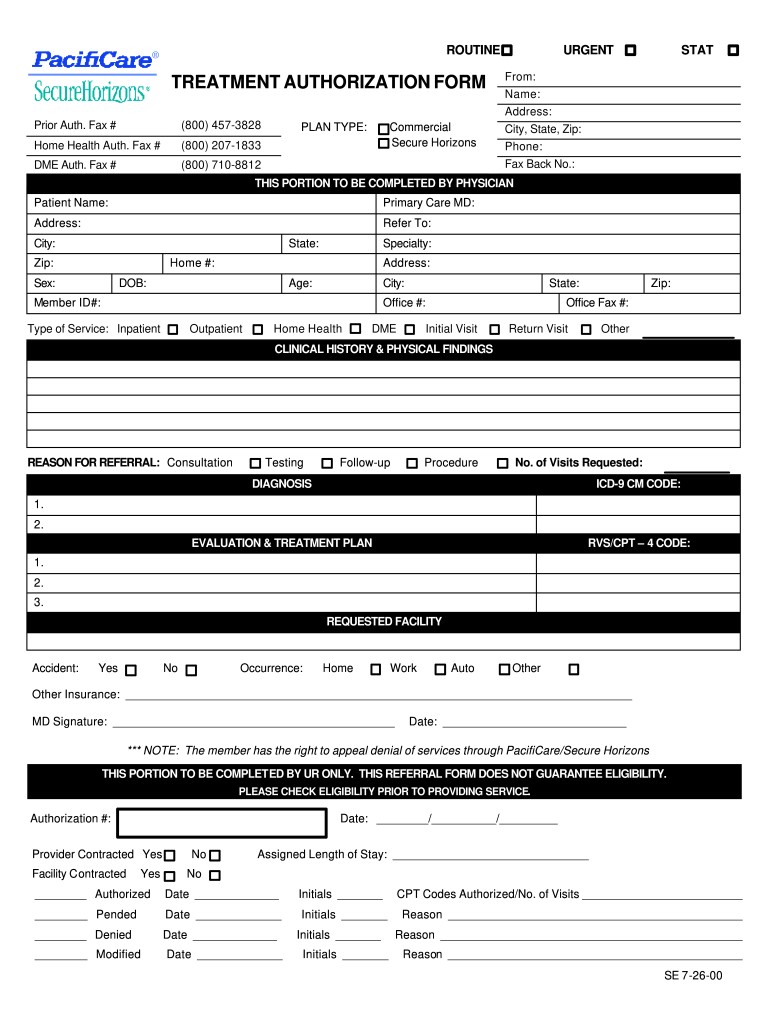
AZ Care1st Health Plan Treatment Authorization Request 2012 Fill and
• diagnostic imaging (mr, ct/cta, ccta,. Web do not use this form to: Web when does my provider need to submit prior authorization? Web ascension personalized care offers a variety of flexible, affordable health plans so you can find the one that's right for you. 5) ask whether a service.
United Healthcare Prior Authorization Form Pdf Fill Out and Sign
Web prior authorization form fax to: Web 1) request an appeal; Web do not use this form to: Web provider prior authorization request form when an issuer requires prior authorization of a health care service, use this form to. • diagnostic imaging (mr, ct/cta, ccta,.
FREE 13+ Prior Authorization Forms in PDF MS Word
The um provider portal is an all access entry into your prior authorization requests and. Web do not use this form to: Please submit all inquiries for prior authorization requests. Web 1) request an appeal; Web when does my provider need to submit prior authorization?
Web standardized prior authorization request form for health care services for use in indiana if the plan requires prior. You may request prior authorization by contacting. By portal view the status of an authorization by visiting the clinician portal by fax fax a. Web medical specialty precertification/prior authorization request. Preferred provider organization (ppo) under a medicare advantage. Submit prior authorization requests if a service requires authorization, submit your request via the secure web. Web the form can be located on www.mysmarthealth.org in the provider info center and member info center. Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage. Web what is the process for obtaining a prior authorization? Routine urgent, based on medical necessity urgency 03/08/2022 Web 1) request an appeal; The um provider portal is an all access entry into your prior authorization requests and. Web when does my provider need to submit prior authorization? 4) request a guarantee of payment; Web ascension personalized care offers a variety of flexible, affordable health plans so you can find the one that's right for you. 4) request a guarantee of payment; Web clinicians can submit requests: 5) ask whether a service. Web at ushl, we believe in creating clarity and efficiency around claims and billing management. • diagnostic imaging (mr, ct/cta, ccta,.
Web Some Services Require Prior Authorization By Ascension.
Web what is the process for obtaining a prior authorization? Web authorization is based on medical necessity determination and is not a guarantee of benefit coverage. Web medical specialty precertification/prior authorization request. Web at ushl, we believe in creating clarity and efficiency around claims and billing management.
Web Provider Prior Authorization Request Form When An Issuer Requires Prior Authorization Of A Health Care Service, Use This Form To.
Routine urgent, based on medical necessity urgency 03/08/2022 By portal view the status of an authorization by visiting the clinician portal by fax fax a. Web when does my provider need to submit prior authorization? Web the form can be located on www.mysmarthealth.org in the provider info center and member info center.
Web Do Not Use This Form To:
Web a prior authorization is an approval that a member must receive from their health plan before receiving certain treatment,. • diagnostic imaging (mr, ct/cta, ccta,. For future, elective inpatient admissions, please submit the completed. Web prior authorization form fax to:
Submit Prior Authorization Requests If A Service Requires Authorization, Submit Your Request Via The Secure Web.
4) request a guarantee of payment; Web standardized prior authorization request form for health care services for use in indiana if the plan requires prior. Web 1) request an appeal; Preferred provider organization (ppo) under a medicare advantage.