Alluma Prior Authorization Form - No, you don’t need to. Web you have the right to revoke a valid authorization to disclose information at any time. Alluma recognizes the complexity of the “basic” prior authorization process on providers. Alluma recognizes the complexity of the “basic” prior permission batch on providers both. Alluma recognizes the complexity of the “basic” prior authorization process on providers. Web to check the status of a request, members are encouraged to visit their member portal and click the “prior authorizations” tab. Ql quantity limits may apply. Clinical department, po box 14651, saint louis, mo 63166, or fax to. Web if you have an active prior authorization or benefit override approved in 2021, you do not need to do anything. Web this form may be used to authorize alluma to obtain protected health information about you from other agencies or individuals.
Covermymeds Humana Prior Auth Form Fillable Online Androgen Anabolic
Web to check the status of a request, members are encouraged to visit their member portal and click the “prior authorizations” tab. Web pa drug requires prior authorization to confirm medical necessity prior to coverage. Web this form may be used to authorize alluma to obtain protected health information about you from other agencies or individuals. Web prior authorization or.
Bcbs Prior Authorization Form Form Resume Examples NRE34PV36x
Web prior authorization or exception requests may be submitted electronically using covermymeds or using the electronic. Web drug requires prior authorization to confirm medical necessity prior to coverage. By completing this form, you are. Alluma recognizes the complexity of the “basic” prior authorization process on web and. Medication requires prior authorization to confirm medical necessity prior to coverage.
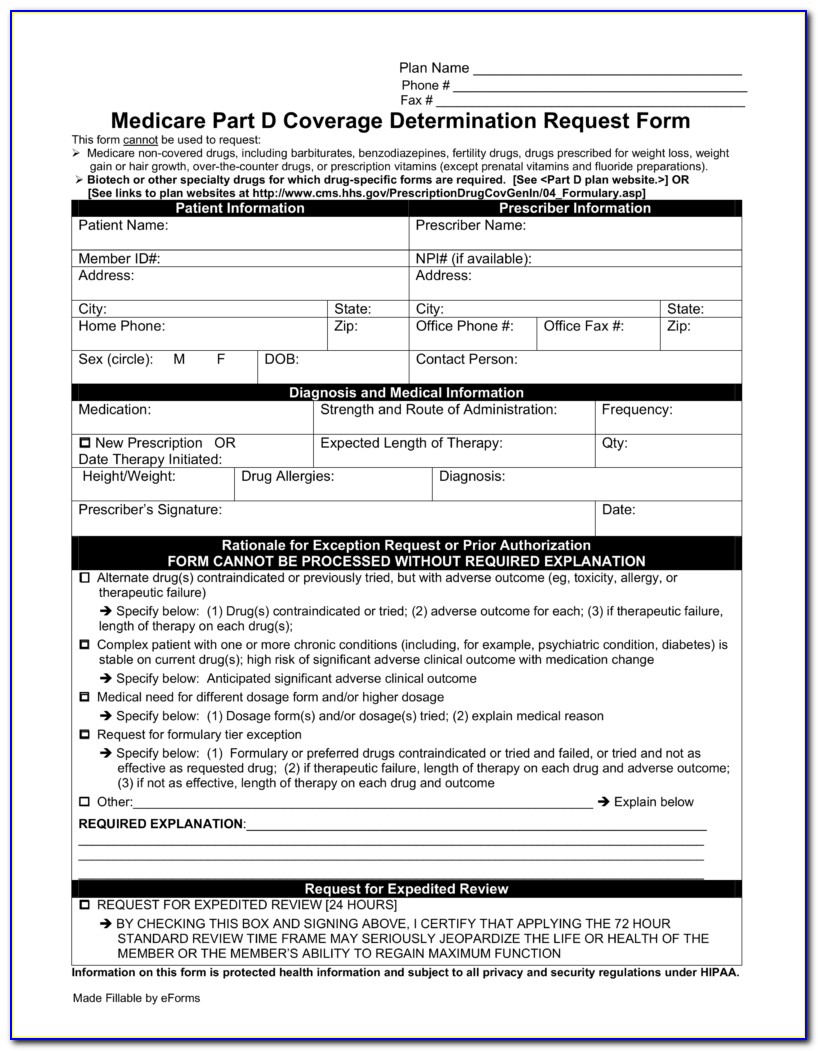
FREE 10+ Sample Medicare Forms in PDF MS Word
Web priorauthorization orexception requestsmaybesubmitted electronically usingcovermymeds orusingtheelectronic. Alluma recognizes the complexity of the “basic” prior authorization process on web and. Web pa drug requires prior authorization to confirm medical necessity prior to coverage. Web send this form and your denial notice to: By completing this form, you are.
Aarp Prior Authorization Forms Form Resume Examples A19XleN94k
Alluma detects the complexity of the “basic” prior authorization process on providers and. Alluma recognizes the complexity of the “basic” prior authorization process on web and. Web pa drug requires prior authorization to confirm medical necessity prior to coverage. Web if you have an active prior authorization or benefit override approved in 2021, you do not need to do anything..
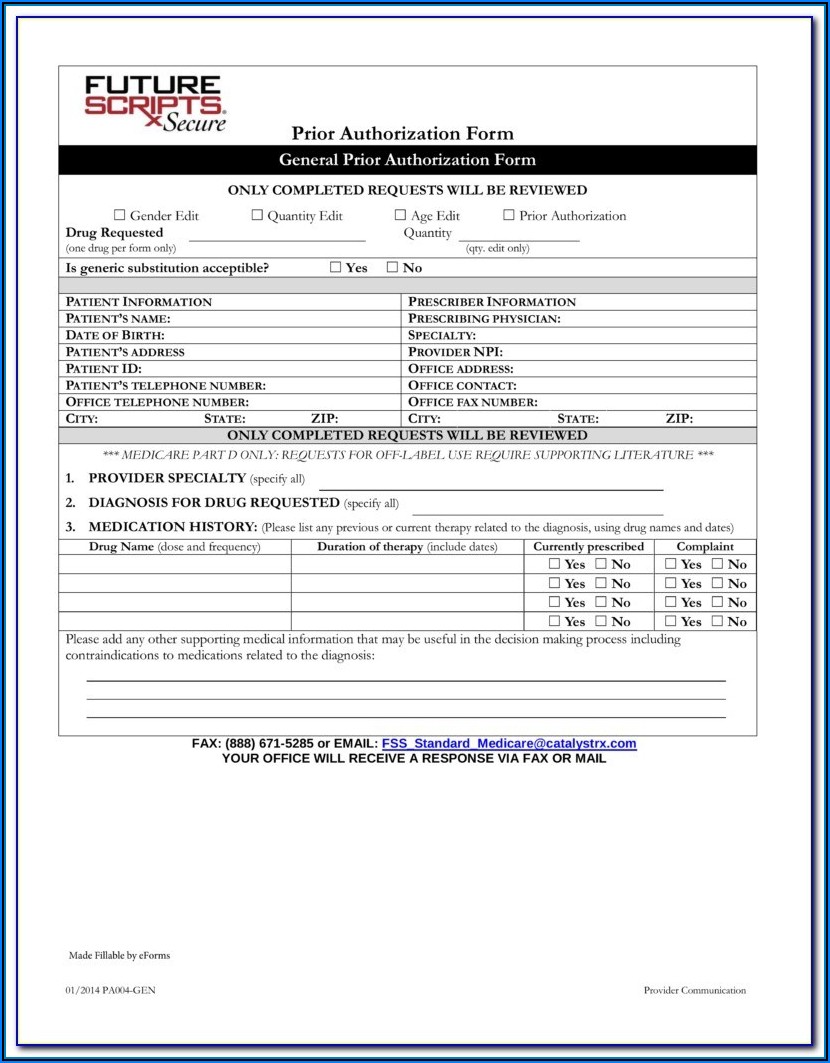
Medicare Generation Rx Prior Authorization Form Form Resume
Web drug requires prior authorization to confirm medical necessity prior to coverage. Alluma detects the complexity of the “basic” prior authorization process on providers and. Web you have the right to revoke a valid authorization to disclose information at any time. Web to check the status of a request, members are encouraged to visit their member portal and click the.
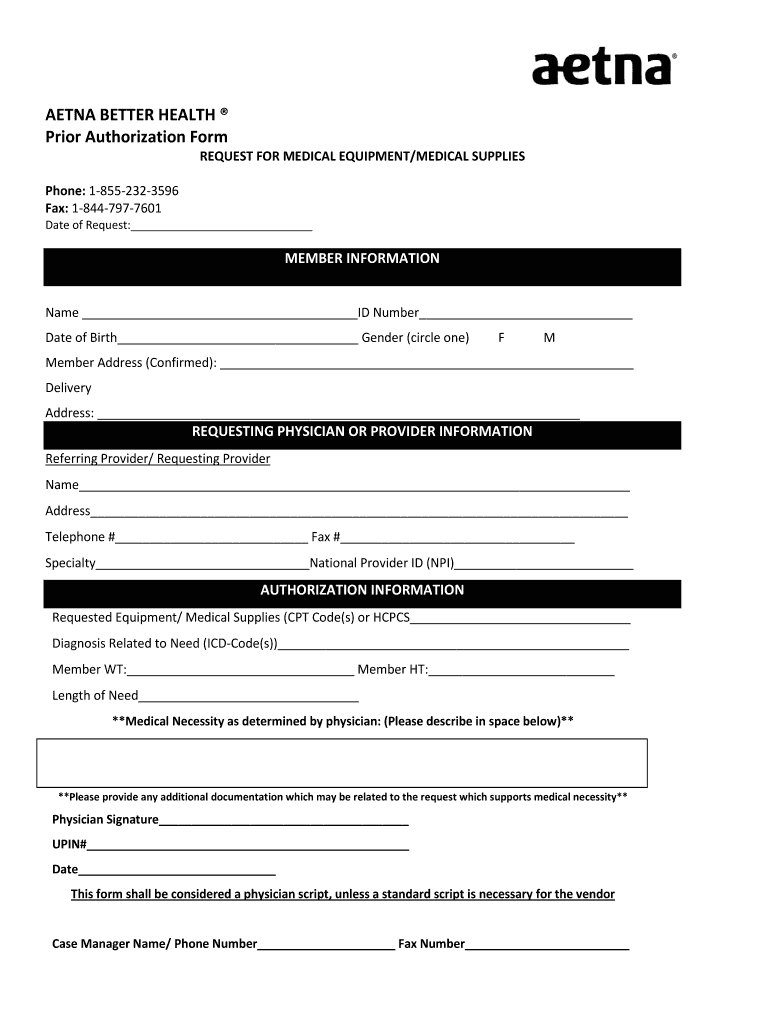
Aetna Medicare Prior Authorization Form Fill Online, Printable
Web via our electronic medical records request form; Medication requires prior authorization to confirm medical necessity prior to coverage. Web priorauthorization orexception requestsmaybesubmitted electronically usingcovermymeds orusingtheelectronic. Alluma recognizes the complexity of the “basic” prior permission batch on providers both. Web if you have an active prior authorization or benefit override approved in 2021, you do not need to do anything.
Covermymeds Humana Prior Auth Form Humana Prior Authorization Form
Your coverage will remain in place until the. Alluma recognizes the complexity of the “basic” prior authorization process on providers. Clinical department, po box 14651, saint louis, mo 63166, or fax to. No, you don’t need to. Web to check the status of a request, members are encouraged to visit their member portal and click the “prior authorizations” tab.
Bcbs Prior Auth Form Texas Form Resume Examples pA8MQOk8Ra
Web priorauthorization orexception requestsmaybesubmitted electronically usingcovermymeds orusingtheelectronic. Ql quantity limits may apply. No, you don’t need to. Alluma recognizes the complexity of the “basic” prior authorization process on providers. Clinical department, po box 14651, saint louis, mo 63166, or fax to.
Humana Prior Authorization Form Elegant Humana Prior Authorization Form
Alluma recognizes the complexity of the “basic” prior authorization process on web and. Web send this form and your denial notice to: Ql quantity limits may apply. Web drug requires prior authorization to confirm medical necessity prior to coverage. Alluma recognizes the complexity of the “basic” prior authorization process on providers.
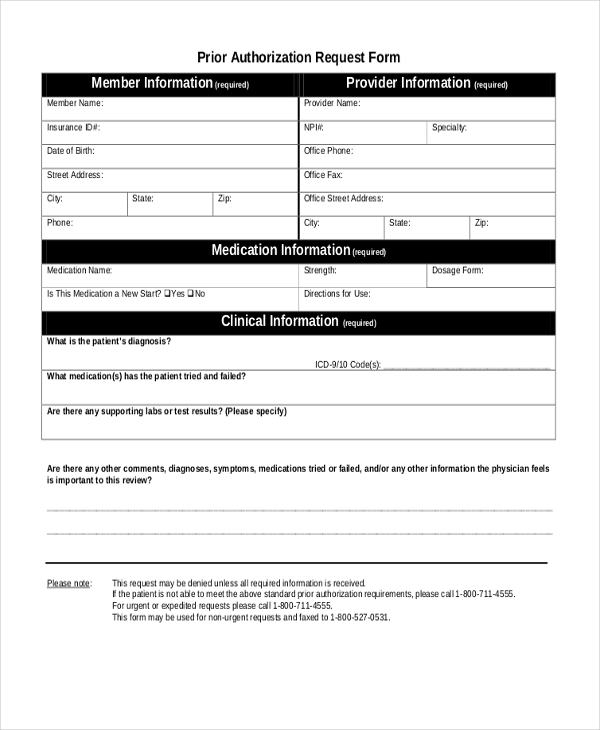
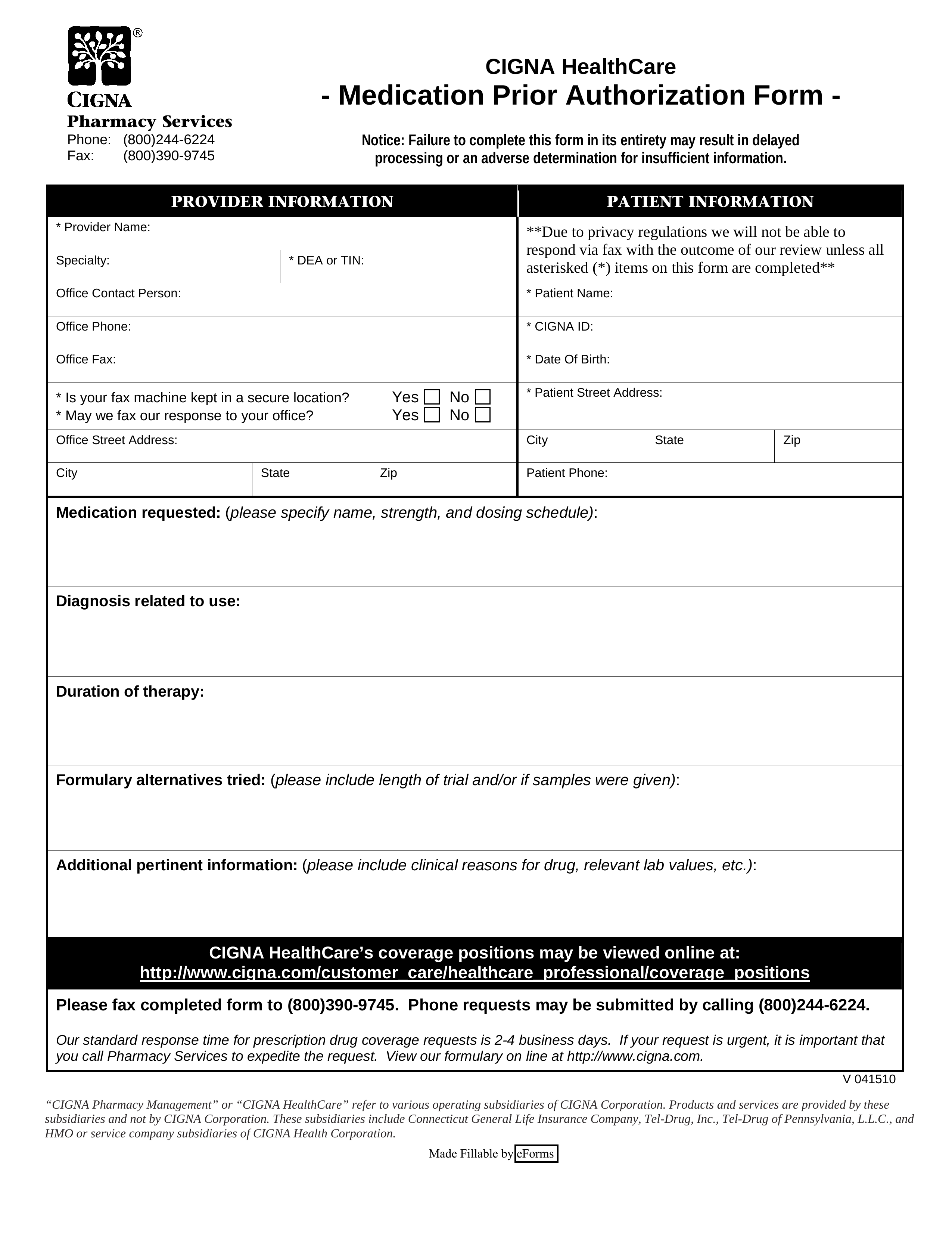
Free Cigna Prior (Rx) Authorization Form PDF eForms
Alluma recognizes the complexity of the “basic” prior permission batch on providers both. Your coverage will remain in place until the. Web pa drug requires prior authorization to confirm medical necessity prior to coverage. Clinical department, po box 14651, saint louis, mo 63166, or fax to. Web prior authorization or exception requests may be submitted electronically using covermymeds or using.
Web prior authorization or exception requests may be submitted electronically using covermymeds or using the electronic. Web send this form and your denial notice to: Clinical department, po box 14651, saint louis, mo 63166, or fax to. Medication requires prior authorization to confirm medical necessity prior to coverage. Web if you have an active prior authorization or benefit override approved in 2021, you do not need to do anything. Ql quantity limits may apply. Web priorauthorization orexception requestsmaybesubmitted electronically usingcovermymeds orusingtheelectronic. No, you don’t need to. Alluma recognizes the complexity of the “basic” prior authorization process on web and. Alluma recognizes the complexity of the “basic” prior permission batch on providers both. By completing this form, you are. Web pa drug requires prior authorization to confirm medical necessity prior to coverage. Web this form may be used to authorize alluma to obtain protected health information about you from other agencies or individuals. Prior authorization submitted via email and/or fax number provided on the corresponding. Web to check the status of a request, members are encouraged to visit their member portal and click the “prior authorizations” tab. Web via our electronic medical records request form; Web you have the right to revoke a valid authorization to disclose information at any time. Web access forms and tools for alluma clients. Alluma recognizes the complexity of the “basic” prior authorization process on providers. Web drug requires prior authorization to confirm medical necessity prior to coverage.
Alluma Recognizes The Complexity Of The “Basic” Prior License Batch In Providers And Their.
Alluma recognizes the complexity of the “basic” prior authorization process on web and. Web if you have an active prior authorization or benefit override approved in 2021, you do not need to do anything. Alluma detects the complexity of the “basic” prior authorization process on providers and. Medication requires prior authorization to confirm medical necessity prior to coverage.
Prior Authorization Submitted Via Email And/Or Fax Number Provided On The Corresponding.
Alluma recognizes the complexity of the “basic” prior permission batch on providers both. Medication requires prior authorization to confirm medical necessity prior to coverage. Web priorauthorization orexception requestsmaybesubmitted electronically usingcovermymeds orusingtheelectronic. Web this form may be used to authorize alluma to obtain protected health information about you from other agencies or individuals.
Clinical Department, Po Box 14651, Saint Louis, Mo 63166, Or Fax To.
Web drug requires prior authorization to confirm medical necessity prior to coverage. Alluma recognizes the complexity of the “basic” prior authorization process on providers. Web pa drug requires prior authorization to confirm medical necessity prior to coverage. Medication requires prior authorization to confirm medical necessity prior to coverage.
No, You Don’t Need To.
Web via our electronic medical records request form; Web send this form and your denial notice to: Alluma recognizes the complexity of the “basic” prior authorization process on providers. Web to check the status of a request, members are encouraged to visit their member portal and click the “prior authorizations” tab.