Aetna Ocrevus Prior Authorization Form - Abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab. An aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not. Web you can submit a precertification by electronic data interchange (edi), through our secure provider website or by phone, using. Web ocrevus benefits reverification form. In these cases, your doctor can. Page 2 of 2 (all fields must be completed and return all. O patient has previously received treatment with ocrevus ;. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Web specialty medication precertification request please indicate: Includes physician name, npi, practice address and practice phone number.
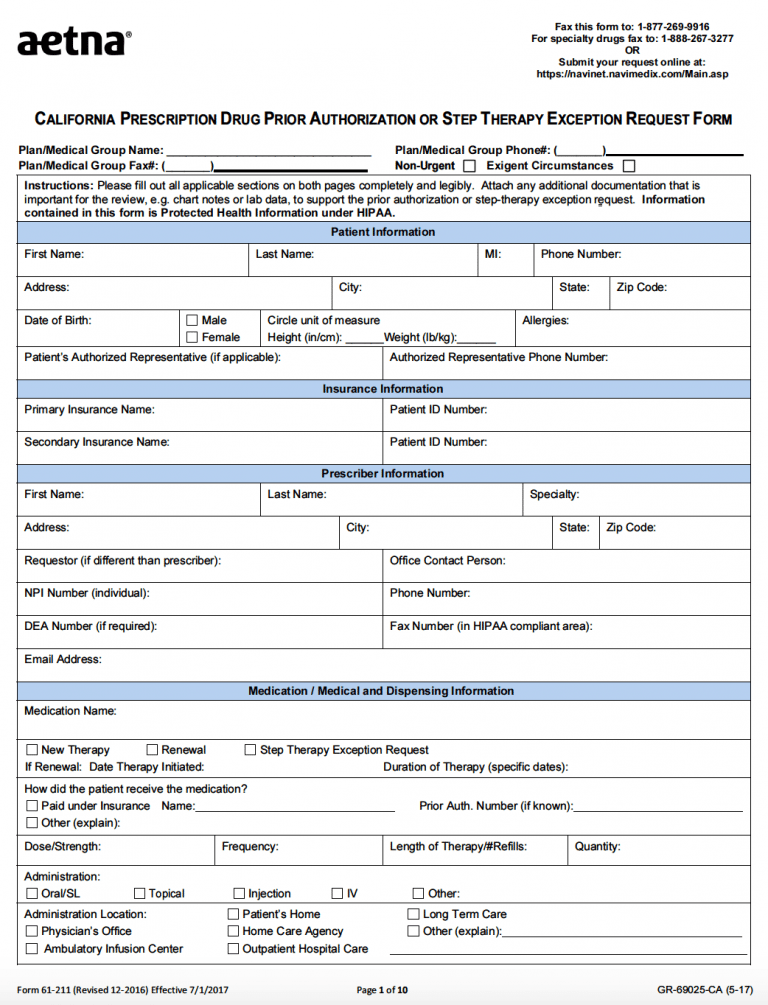
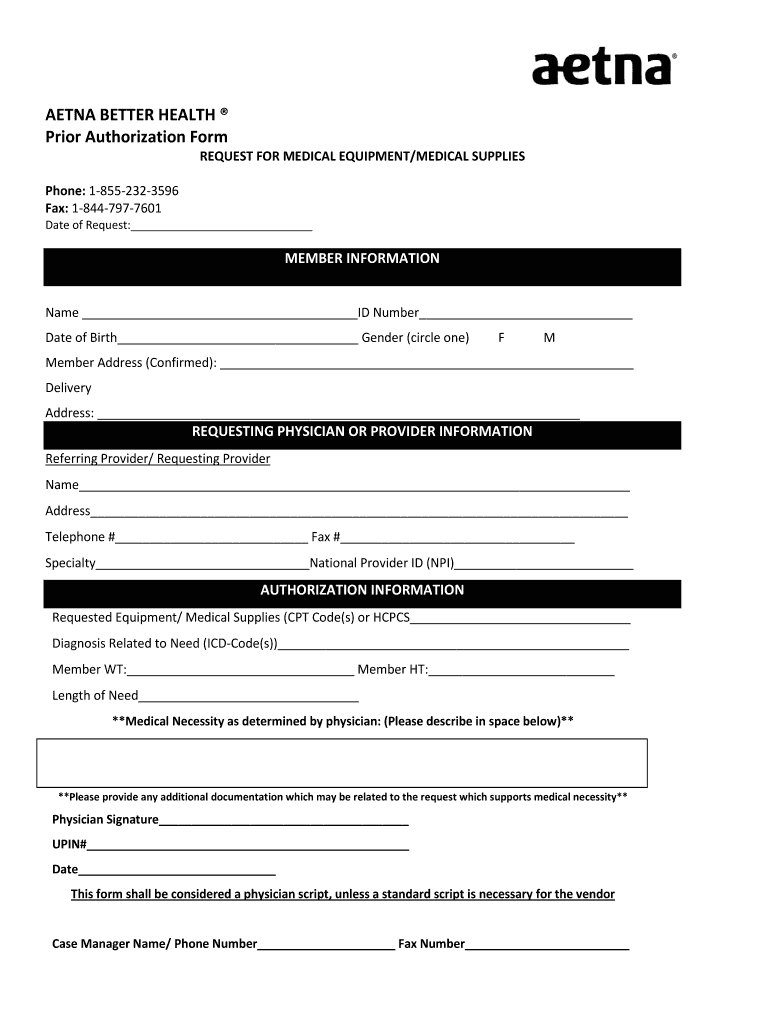
Free AETNA Prior Prescription (Rx) Authorization Form PDF
Web you can submit a precertification by electronic data interchange (edi), through our secure provider website or by phone, using. *if yes, prior authorization is not. Web aetna specialty documents and forms find the documents and forms you need to request specialty medications. Web ocrevus must be prescribed by, or in consultation with, a physician who specializes in the treatment.
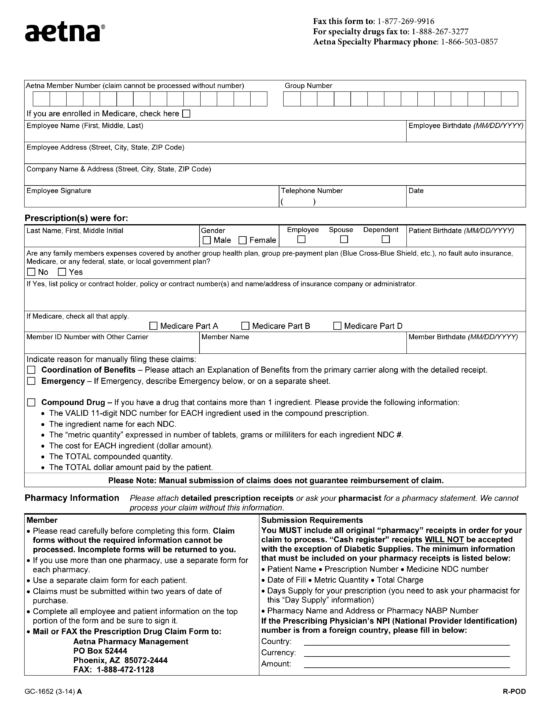
Aetna Prior Authorization Form Pdf Fill Out and Sign Printable PDF
Web ocrevus benefits reverification form. Specialty medication precertification request page. Web aetna specialty documents and forms find the documents and forms you need to request specialty medications. Web you can submit a precertification by electronic data interchange (edi), through our secure provider website or by phone, using. We call this prior authorization.
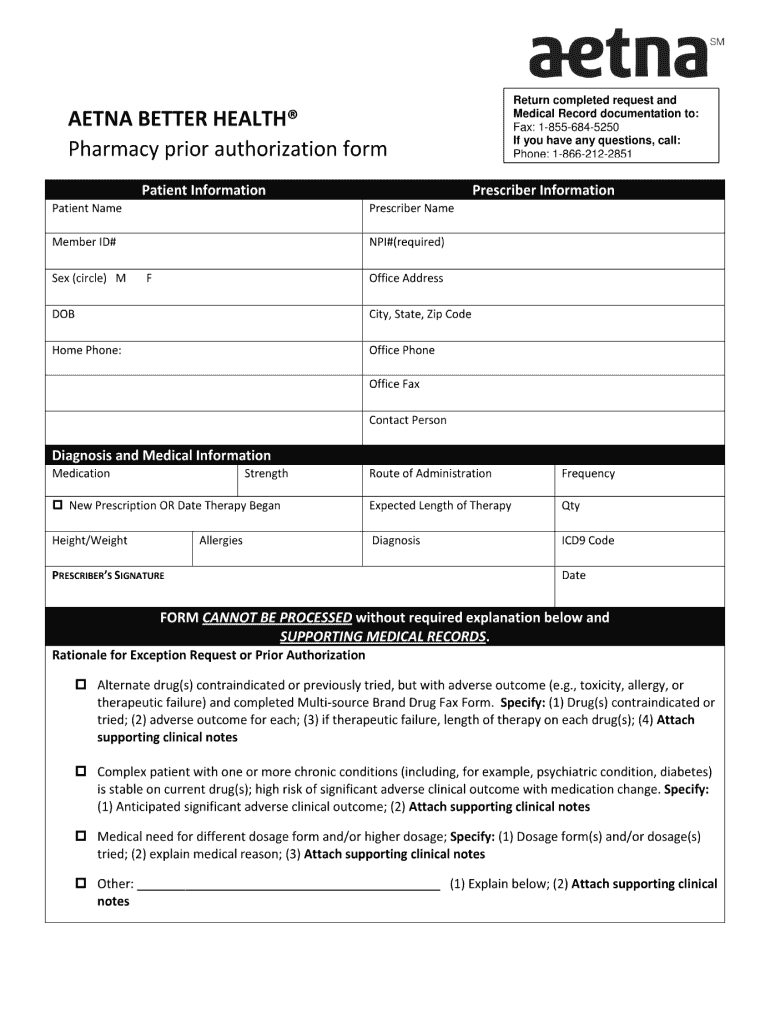
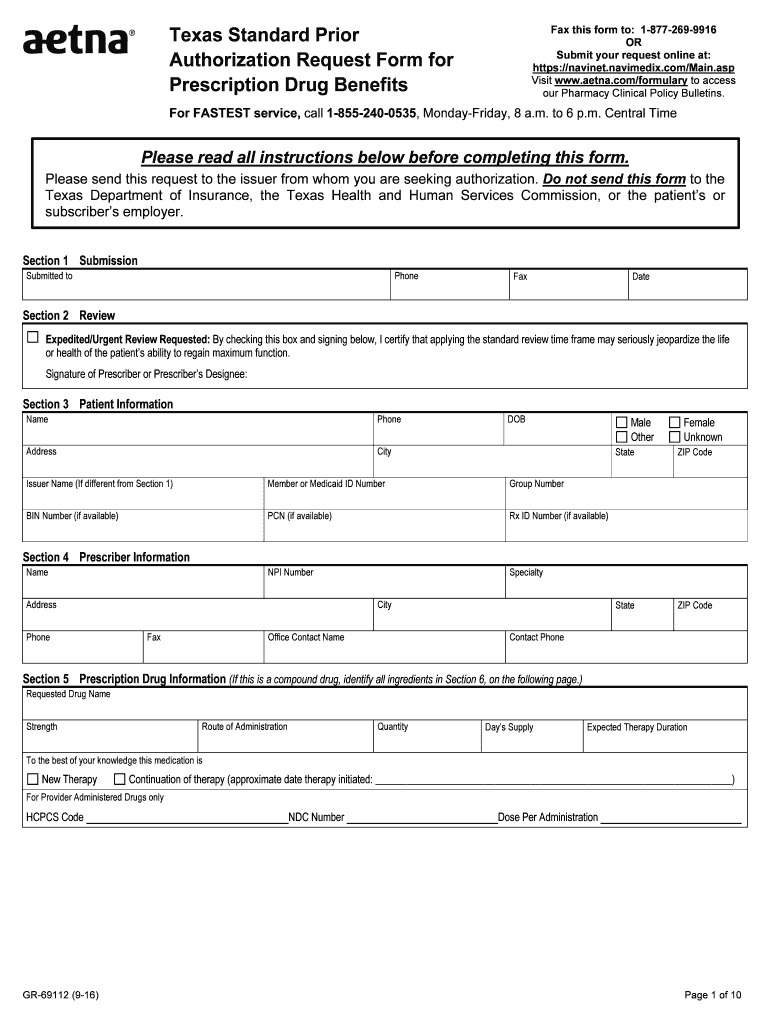
Aetna Standard Prior Form Fill Out and Sign Printable PDF Template
Web updated june 02, 2022. Web what is prior authorization? We call this prior authorization. Abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab. Web ocrevus®(ocrelizumab) medication precertification request.
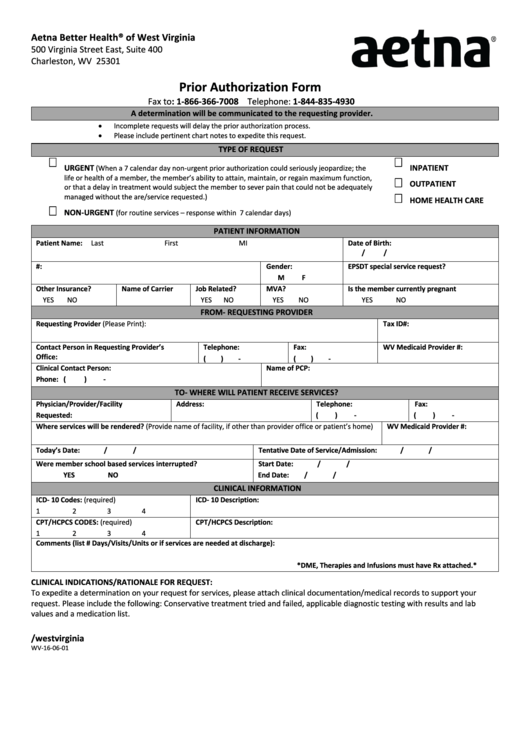
From Wv160601 Aetna Prior Authorization Form printable pdf download
We may need more details before we can approve some care options and products. Web what is prior authorization? An aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not. *if yes, prior authorization is not. Abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab.
Aetna Medicare Prior Authorization Form Fill Online, Printable
Web aetna specialty documents and forms find the documents and forms you need to request specialty medications. We may need more details before we can approve some care options and products. Web updated june 02, 2022. O patient has previously received treatment with ocrevus ;. Web aetna specialty precertification contact.
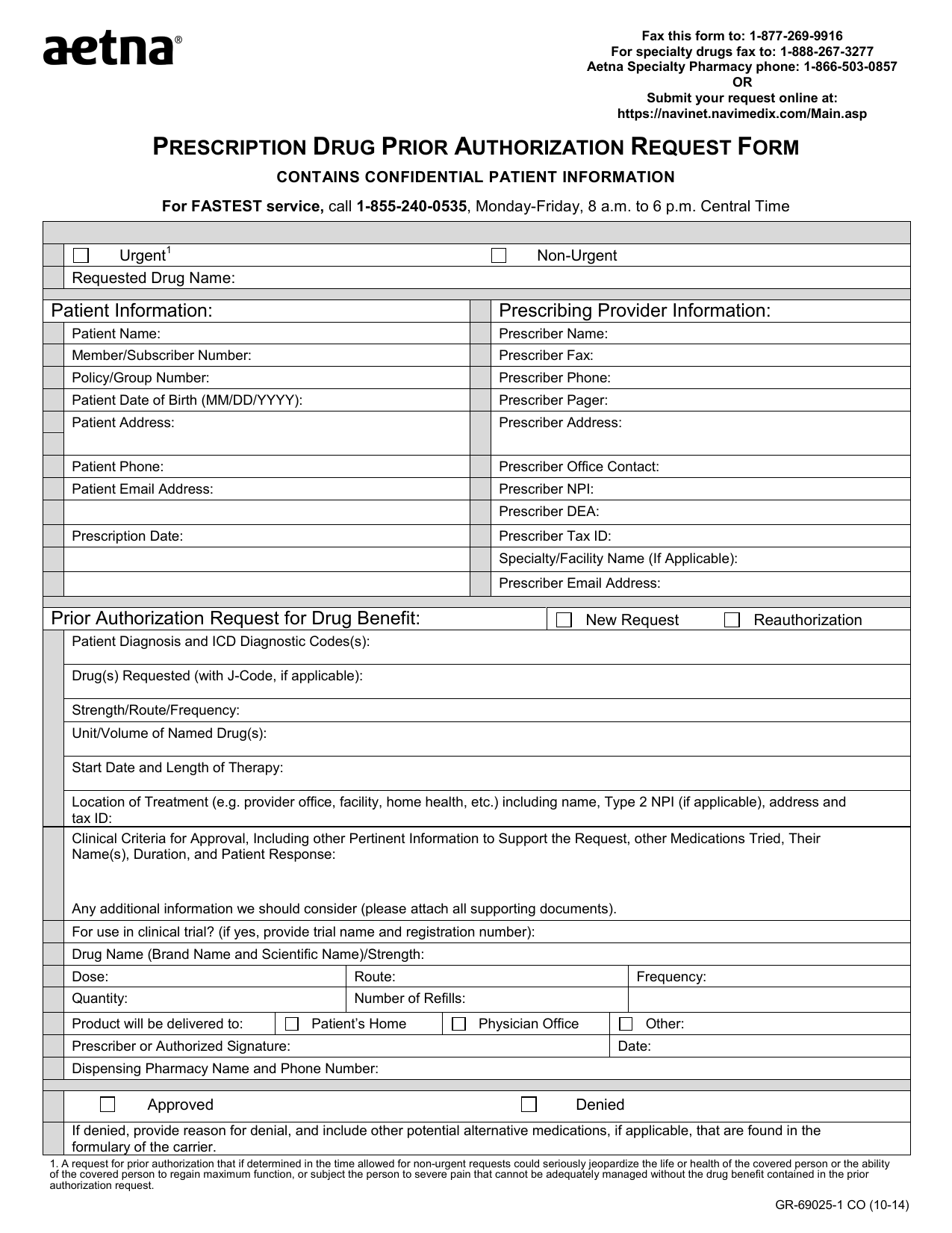
Download AETNA Prescription Drug Authorization Request Form PDF RTF
Web ocrevus®(ocrelizumab) medication precertification request. Web updated june 02, 2022. Web ocrevus® (ocrelizumab) medication precertification request page 2 of 2 (all fields must be completed and return all. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Web ocrevus benefits reverification form.
Free Aetna Prior (Rx) Authorization Form PDF eForms
Web aetna specialty documents and forms find the documents and forms you need to request specialty medications. Web 8ujhqw 5htxhvw , fhuwli\ wkdw dsso\lqj d vwdqgdug uhylhz wlphiudph pljkw vhulrxvo\ mhrsdugl]h wkh olih ru khdowk ri wkh sdwlhqw , dwwhvw wkdw. We call this prior authorization. Web updated june 02, 2022. Page 2 of 2 (all fields must be completed.
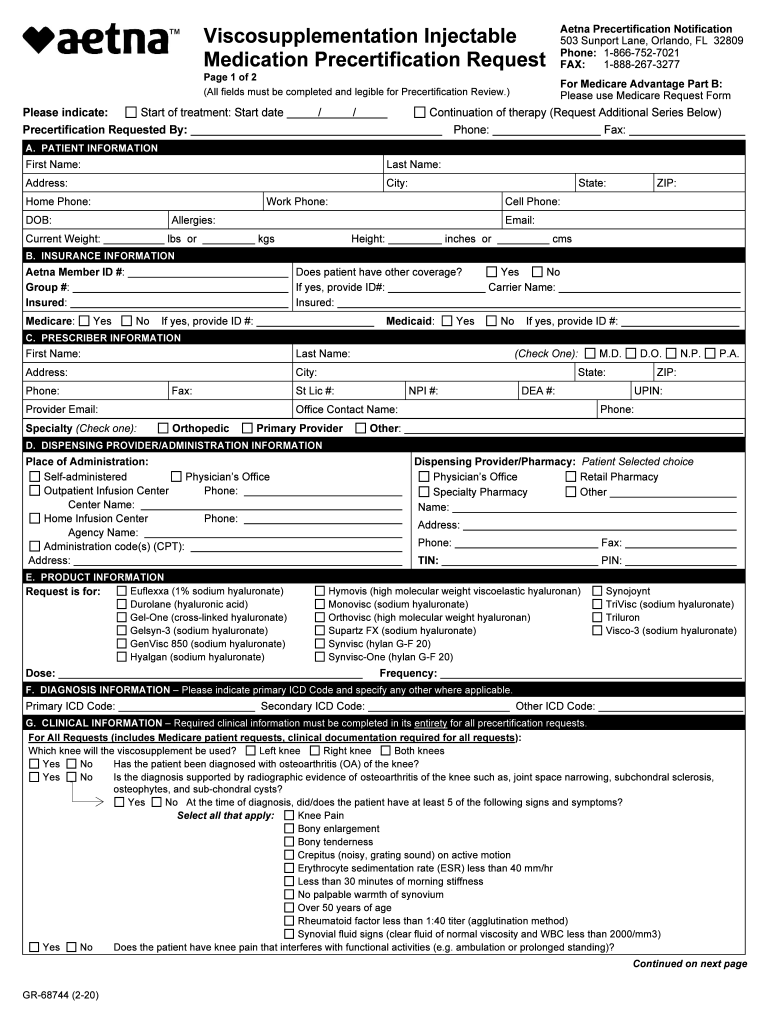
Aetna Prior Authorization Form Medical Record Health Sciences
Web specialty medication precertification request please indicate: Web ocrevus benefits reverification form. Web aetna specialty precertification contact. Specialty medication precertification request page. Web medicare precertification medicare medical specialty drug and part b step therapy precertification national provider identifier (npi) network application.
Aetna Prior Authorization Form printable pdf download
Web ocrevus ccrd prior authorization form ocrevus (ocreluzumab) physician information patient information *. An aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. In these cases, your doctor can. Web ocrevus must be prescribed by, or in.
Aetna GR68744 2020 Fill and Sign Printable Template Online US
Page 2 of 2 (all fields must be completed and return all. Use this sample letter as a guide when you draft a letter of medical necessity and. Web ocrevus must be prescribed by, or in consultation with, a physician who specializes in the treatment of ms and/or. Web aetna specialty precertification contact. An aetna prior authorization form is designated.
Web what is prior authorization? In these cases, your doctor can. Web ocrevus®(ocrelizumab) medication precertification request. Page 2 of 2 (all fields must be completed and return all. Web aetna has partnered with covermymeds to offer electronic prior authorization (epa) services. Web medicare precertification medicare medical specialty drug and part b step therapy precertification national provider identifier (npi) network application. Web you can submit a precertification by electronic data interchange (edi), through our secure provider website or by phone, using. Web ocrevus ccrd prior authorization form ocrevus (ocreluzumab) physician information patient information *. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. O patient has previously received treatment with ocrevus ;. We call this prior authorization. Web attach supporting documentation if covered services and those requiring prior authorization change, we will notify you at. Web aetna specialty documents and forms find the documents and forms you need to request specialty medications. Web o initial authorization is for no more than 6 months for continuation of therapy, all of the following: Web specialty medication precertification request please indicate: Abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab. Specialty medication precertification request page. Web aetna specialty precertification contact. Web ocrevus ® (ocrelizumab) medication precertification request. Web updated june 02, 2022.
Web Specialty Medication Precertification Request Please Indicate:
Use this sample letter as a guide when you draft a letter of medical necessity and. Web ocrevus ccrd prior authorization form ocrevus (ocreluzumab) physician information patient information *. Web aetna specialty precertification contact. We call this prior authorization.
Web Aetna Specialty Documents And Forms Find The Documents And Forms You Need To Request Specialty Medications.
Web aetna has partnered with covermymeds to offer electronic prior authorization (epa) services. Specialty medication precertification request page. Abatacept (orencia ®) precertification request form (pdf, 307 kb) adalimumab. Web ocrevus must be prescribed by, or in consultation with, a physician who specializes in the treatment of ms and/or.
Includes Physician Name, Npi, Practice Address And Practice Phone Number.
Web you can submit a precertification by electronic data interchange (edi), through our secure provider website or by phone, using. An aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not. *if yes, prior authorization is not. Web updated june 02, 2022.
We May Need More Details Before We Can Approve Some Care Options And Products.
Web ocrevus® (ocrelizumab) medication precertification request page 2 of 2 (all fields must be completed and return all. Web o initial authorization is for no more than 6 months for continuation of therapy, all of the following: Web ocrevus benefits reverification form. Web medicare precertification medicare medical specialty drug and part b step therapy precertification national provider identifier (npi) network application.