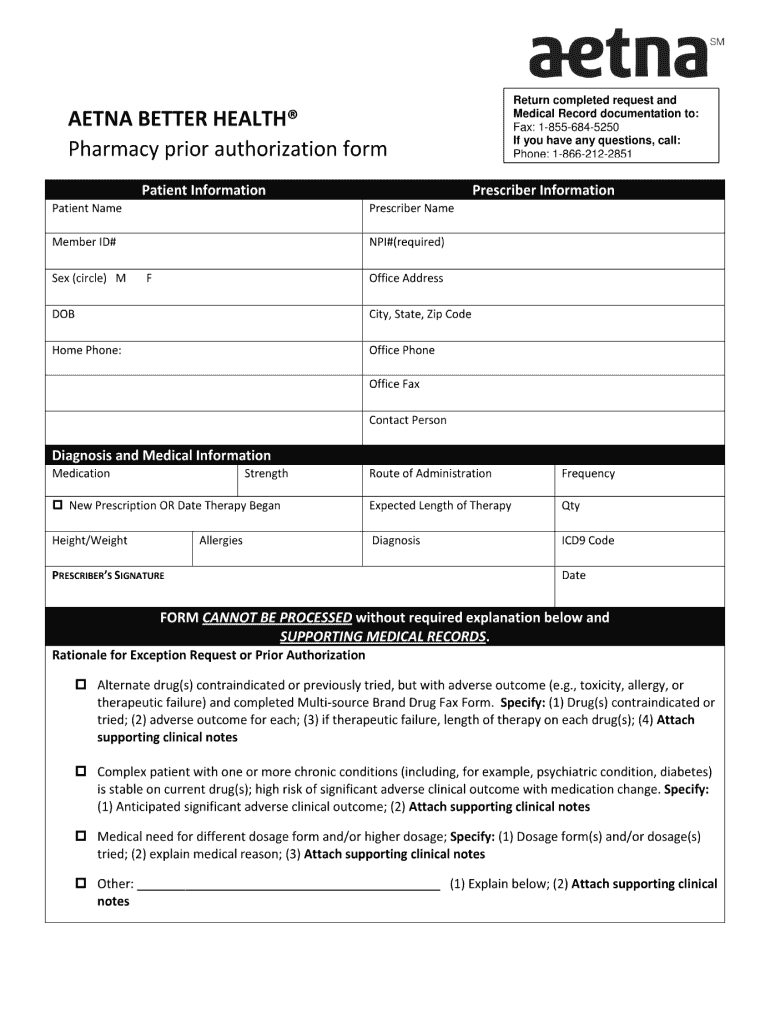
Aetna Entyvio Prior Authorization Form - Web aetna specialty documents and forms find the documents and forms you need to request specialty medications. We may need more details before we can approve some care options and products. Web medicare form entyvio® (vedolizumab) injectable medication precertification request page 3 of 3 (all fields must be. Web initial authorization will be for no more than 14 weeks. Web aetna specialty documents real forms find the documents and forms you need toward please specialty meds. An aetna prior authorization form is designated for medical offices when a particular. Print text, add images, blackout confidential details, added comments, highlights the more. Web aetna prior (rx) authorization form. In these cases, your doctor can. Web find downloadable resources including entyvioconnect enrollment forms, patient education materials, financial assistance forms, and.
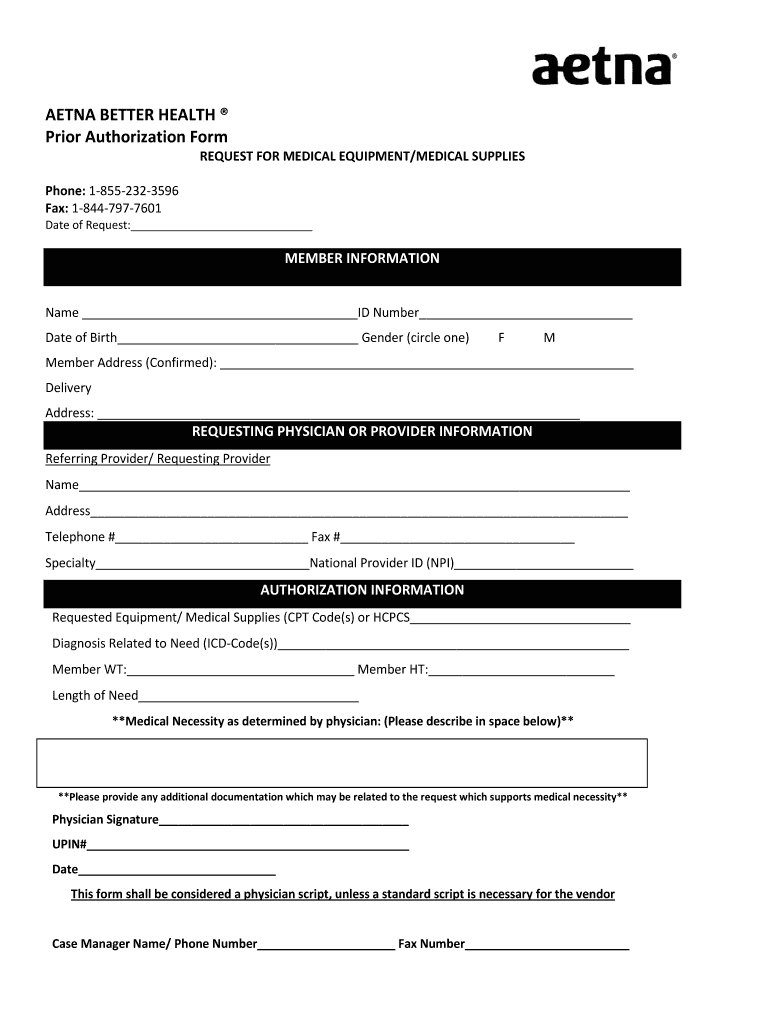
Aetna Medicare Prior Authorization Form Fill Online, Printable
Web medicare form entyvio® (vedolizumab) injectable medication precertification request page 3 of 3 (all fields must be. For medicare advantage part b: Web edit your form online. An aetna prior authorization form is designated for medical offices when a particular. Web aetna specialty documents and forms find the documents and forms you need to request specialty medications.
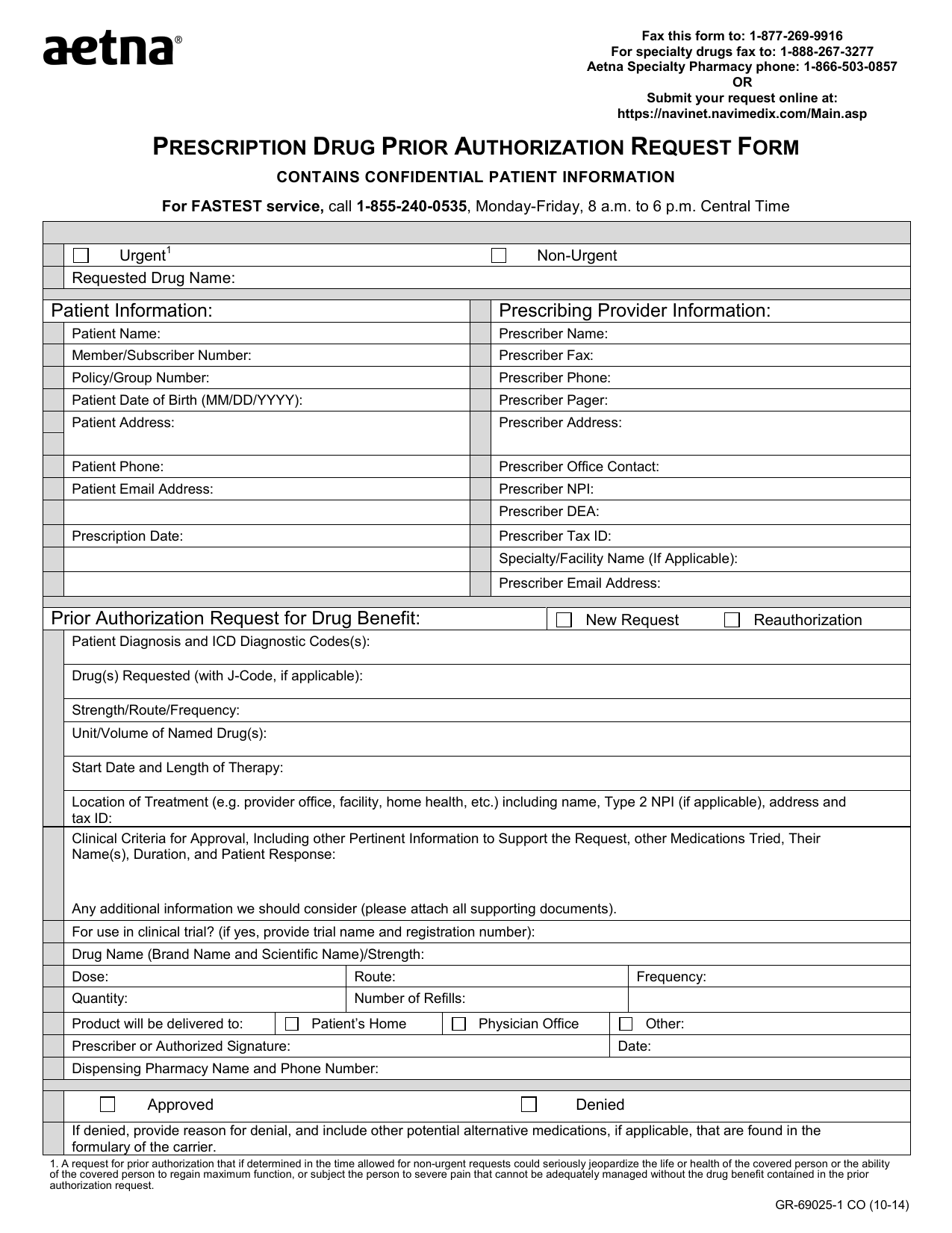
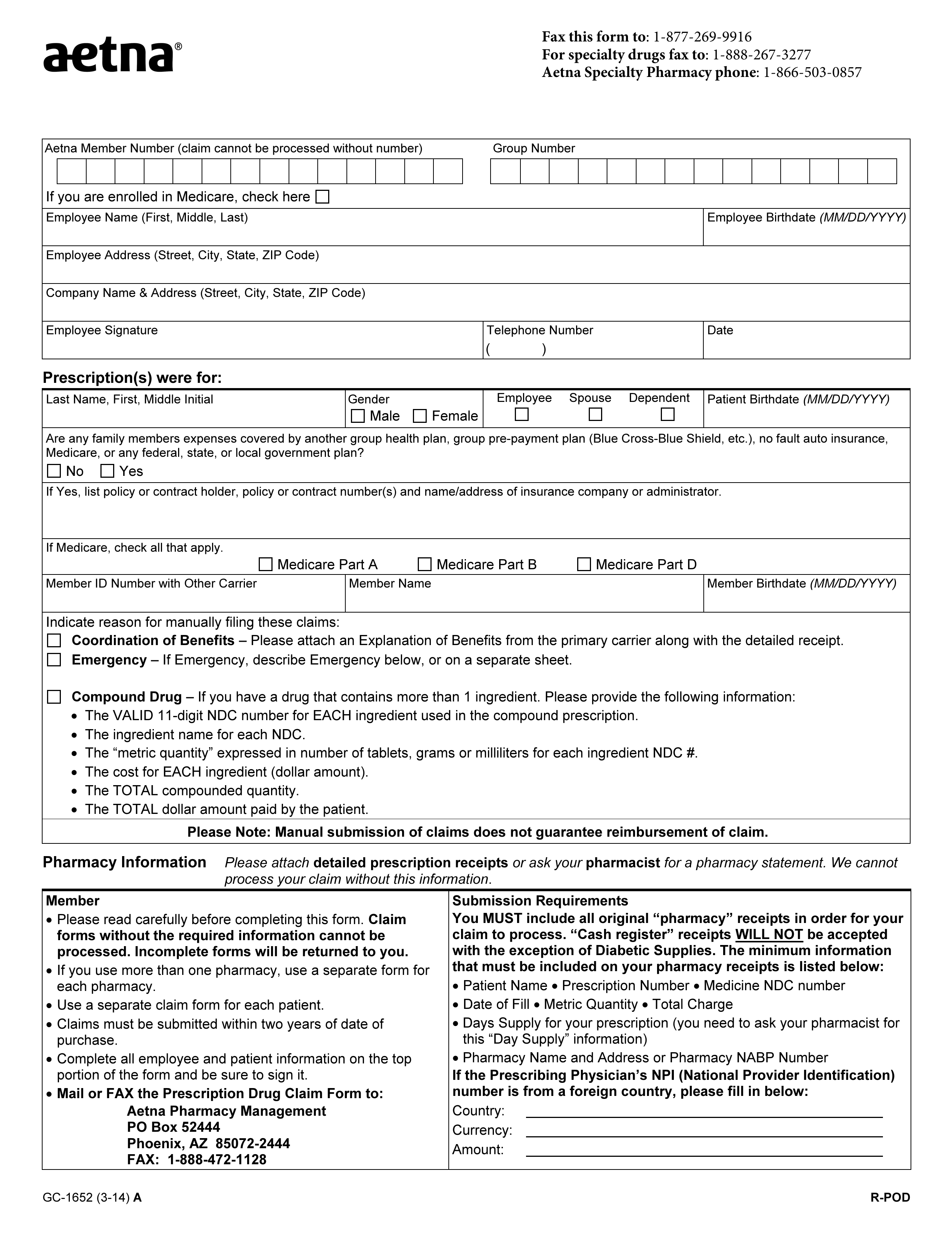
Download AETNA Prescription Drug Authorization Request Form PDF RTF
In these cases, your doctor can. 4) request a guarantee of payment; Web search downloadable resources including entyvioconnect register forms, patient education materials, financial assistance. Web *aetna medicare advantage ppo only covers services approved under traditional medicare and administered by. Web specialty medication precertification request page 1 of 2 (all fields must be completed and legible for precertification review.) start.
Aetna Medicare Medication Prior Authorization Form Form Resume
Web initial authorization will be for no more than 14 weeks. Web do not use this form to: Web entyvio at no cost for up to 1 year while the appeals process is conducted prior authorization (pa) support assistance in. Web aetna specialty documents and forms find the documents and forms you need to request specialty medications. Web precertification of.
NE Aetna GR681894 2018 Fill and Sign Printable Template Online US
Web find forms and applications for health care professionals and patients, all in one place. Web what is prior authorization? Address, phone number and practice changes. Web specialty medication precertification request page 1 of 2 (all fields must be completed and legible for precertification review.) start of treatment: 5) ask whether a service requires prior.
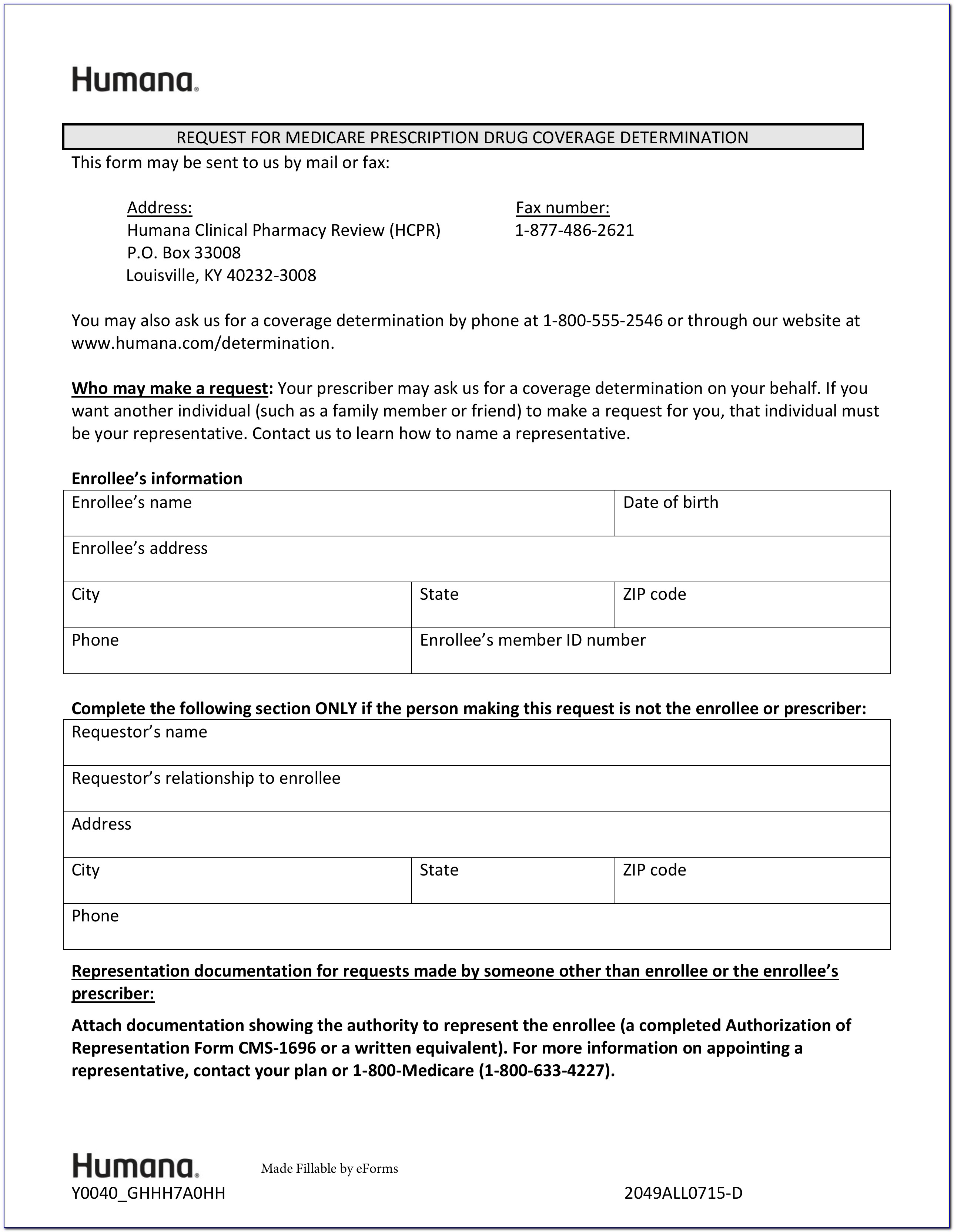
Medicare Part D Medication Prior Authorization Form Form Resume
Web what is prior authorization? O for continuation of therapy , all of the following: Address, phone number and practice changes. Web search downloadable resources including entyvioconnect register forms, patient education materials, financial assistance. Web epo/dialysis medication precertification request form (pdf, 739 kb) etanercept (enbrel ®) precertification request form.
Free Aetna Prior (Rx) Authorization Form PDF eForms
Web entyvio at no cost for up to 1 year while the appeals process is conducted prior authorization (pa) support assistance in. In these cases, your doctor can. Web what is prior authorization? Web find downloadable resources including entyvioconnect enrollment forms, patient education materials, financial assistance forms, and. Web initial authorization will be for no more than 14 weeks.
Aetna Medicare Advantage Disenrollment Form Form Resume Examples
In these cases, your doctor can. Web do not use this form to: O for continuation of therapy , all of the following: During the prior authorization process, it’s reviewed against nationally recognized criteria, the highest. Web medicare form entyvio® (vedolizumab) injectable medication precertification request page 3 of 3 (all fields must be.
Aetna Prior Authorization Form Pdf Fill Out and Sign Printable PDF
Web search downloadable resources including entyvioconnect register forms, patient education materials, financial assistance. Web epo/dialysis medication precertification request form (pdf, 739 kb) etanercept (enbrel ®) precertification request form. Web what is prior authorization? O for continuation of therapy , all of the following: An aetna prior authorization form is designated for medical offices when a particular.
20202022 Form Aetna GR68457 Fill Online, Printable, Fillable, Blank
4) request a guarantee of payment; Print text, add images, blackout confidential details, added comments, highlights the more. Web aetna specialty documents and forms find the documents and forms you need to request specialty medications. We may need more details before we can approve some care options and products. In these cases, your doctor can.
Aetna Specialty Pharmacy Prior Authorization Form PharmacyWalls
Web initial authorization will be for no more than 14 weeks. Web do not use this form to: Web aetna prior (rx) authorization form. Web if your doctor believes you have a specific clinical need for one of these products, he or she should contact the prior authorization department at: An aetna prior authorization form is designated for medical offices.
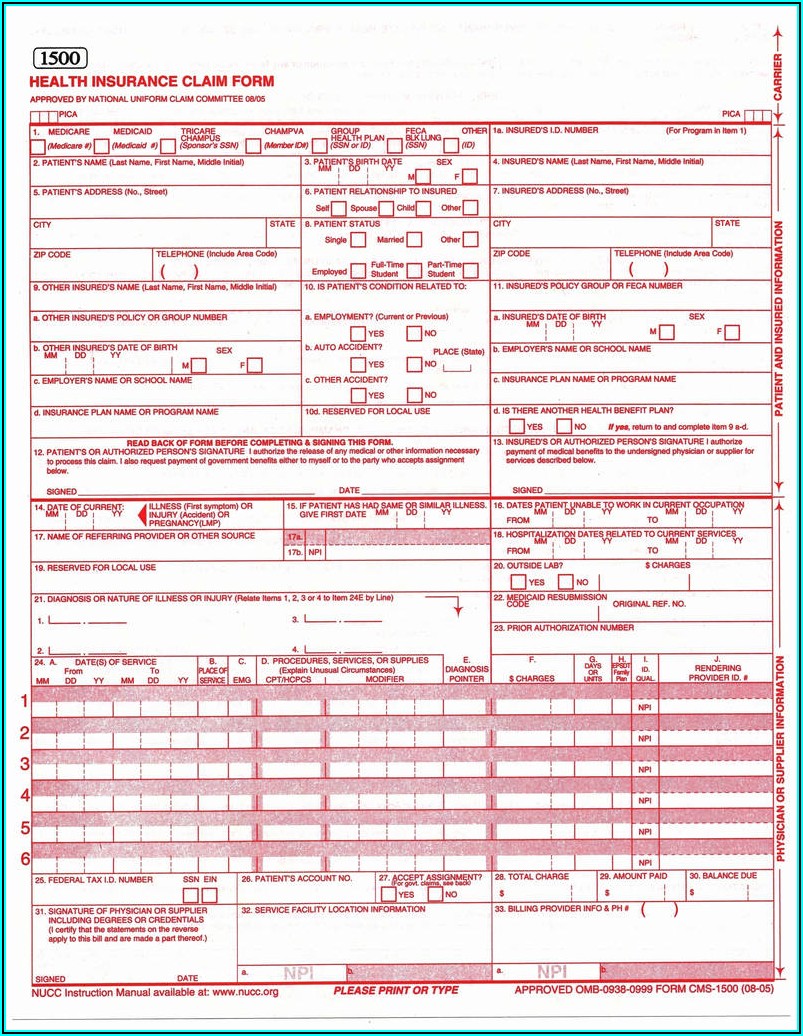
An aetna prior authorization form is designated for medical offices when a particular. O for continuation of therapy , all of the following: Web medicare form entyvio® (vedolizumab) injectable medication precertification request page 3 of 3 (all fields must be. Address, phone number and practice changes. Print text, add images, blackout confidential details, added comments, highlights the more. During the prior authorization process, it’s reviewed against nationally recognized criteria, the highest. Web find forms and applications for health care professionals and patients, all in one place. In these cases, your doctor can. Web if your doctor believes you have a specific clinical need for one of these products, he or she should contact the prior authorization department at: 5) ask whether a service requires prior. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you. Web medicare form entyvio ® (vedolizumab) injectable medication precertification request page 2 of 3 (all fields must be. Web entyvio at no cost for up to 1 year while the appeals process is conducted prior authorization (pa) support assistance in. 4) request a guarantee of payment; We call this prior authorization. Web edit your form online. Web what is prior authorization? We may need more details before we can approve some care options and products. Web aetna prior (rx) authorization form. Web *aetna medicare advantage ppo only covers services approved under traditional medicare and administered by.
Web Precertification Of Vedolizumab (Entyvio) Is Required Of All Aetna Participating Providers And Members In Applicable Plan Designs.
Web if your doctor believes you have a specific clinical need for one of these products, he or she should contact the prior authorization department at: Web medicare form entyvio ® (vedolizumab) injectable medication precertification request page 2 of 3 (all fields must be. Web edit your form online. For medicare advantage part b:
During The Prior Authorization Process, It’s Reviewed Against Nationally Recognized Criteria, The Highest.
Web *aetna medicare advantage ppo only covers services approved under traditional medicare and administered by. Web search downloadable resources including entyvioconnect register forms, patient education materials, financial assistance. O for continuation of therapy , all of the following: Web medicare form entyvio® (vedolizumab) injectable medication precertification request page 3 of 3 (all fields must be.
5) Ask Whether A Service Requires Prior.
Web do not use this form to: An aetna prior authorization form is designated for medical offices when a particular. Web find downloadable resources including entyvioconnect enrollment forms, patient education materials, financial assistance forms, and. Web some procedures, tests and prescriptions need prior approval to be sure they’re right for you.
Web Specialty Medication Precertification Request Page 1 Of 2 (All Fields Must Be Completed And Legible For Precertification Review.) Start Of Treatment:
Web aetna prior (rx) authorization form. Web what is prior authorization? Address, phone number and practice changes. Web initial authorization will be for no more than 14 weeks.