Aetna Benlysta Prior Authorization Form - Web belimumab (benlysta®) injectable medication precertification request (pdf, 366 kb) botulinum toxins medication. That's why we have a team of experts and a variety of help resources to. Web o benlysta is initiated and titrated according to us food and drug administration labeled dosing for sle; Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web view and download provider related prior authorization information at aetna better health of michigan. Web find all the forms you need. We know pa requests are complex. To make an appropriate determination,. Web precertification of belimumab (benlysta) is required of all aetna participating providers and members in applicable plan designs. Find forms and applications for health care professionals and patients, all in one place.
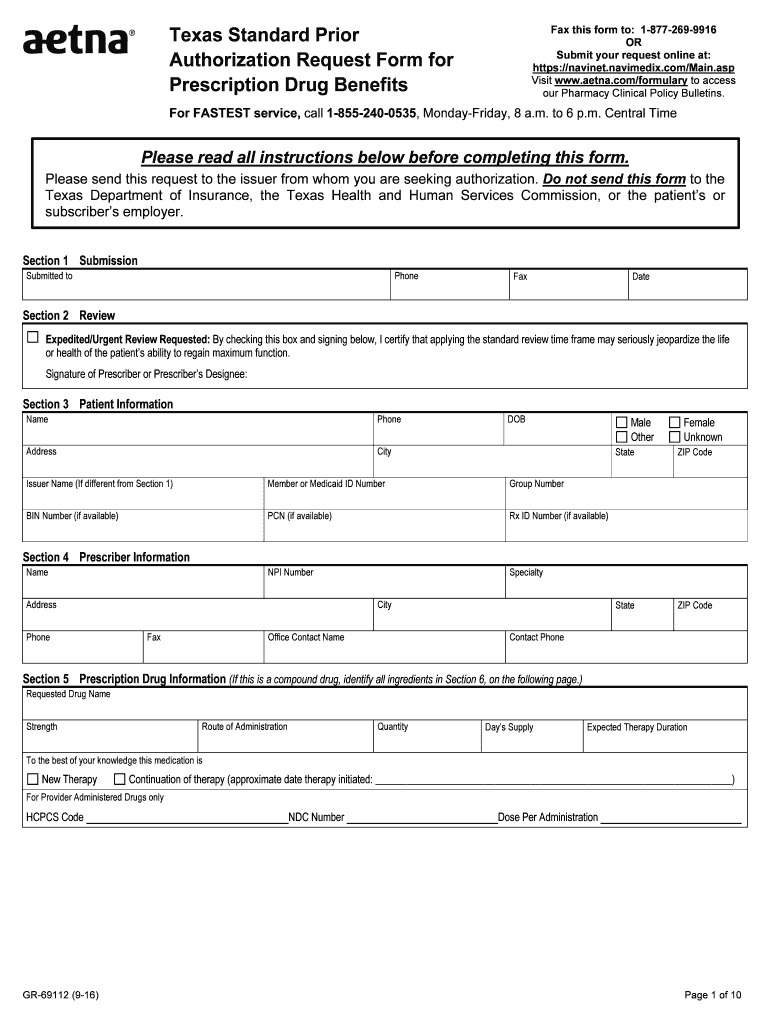
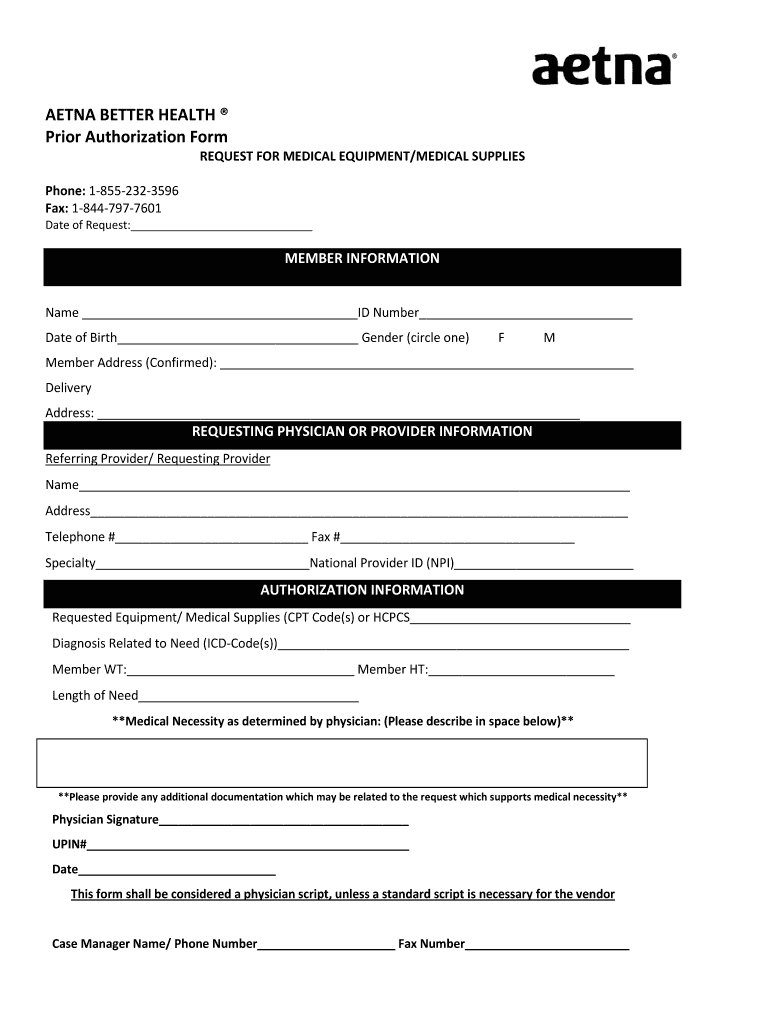
Aetna Standard Prior Form Fill Out and Sign Printable PDF Template
Some procedures, tests and prescriptions need prior approval to be sure they’re right for. Web prior authorization form all fields on this form are required. An aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not. And o initial authorization is for no more than 12 months. Web precertification of belimumab (benlysta) is required.
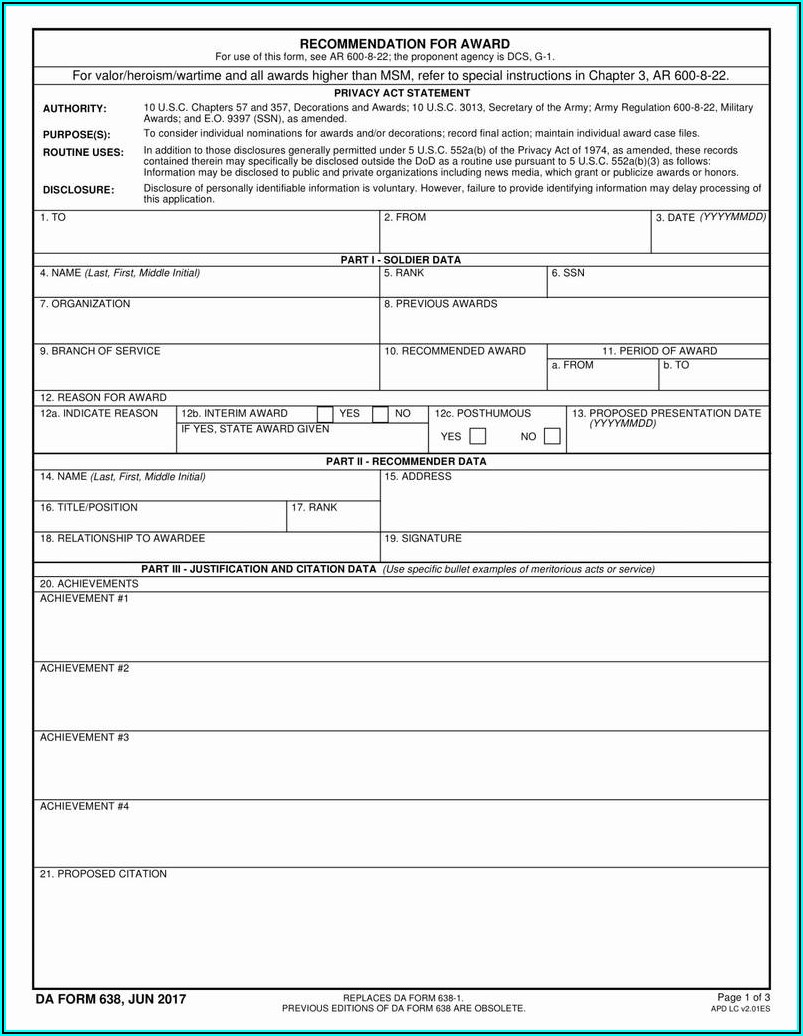
Aetna GR68285 Form 2011 Fill and Sign Printable Template Online US
We call this prior authorization. Web what is prior authorization? An aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not. And o initial authorization is for no more than 12 months. Web o benlysta is initiated and titrated according to us food and drug administration labeled dosing for sle;
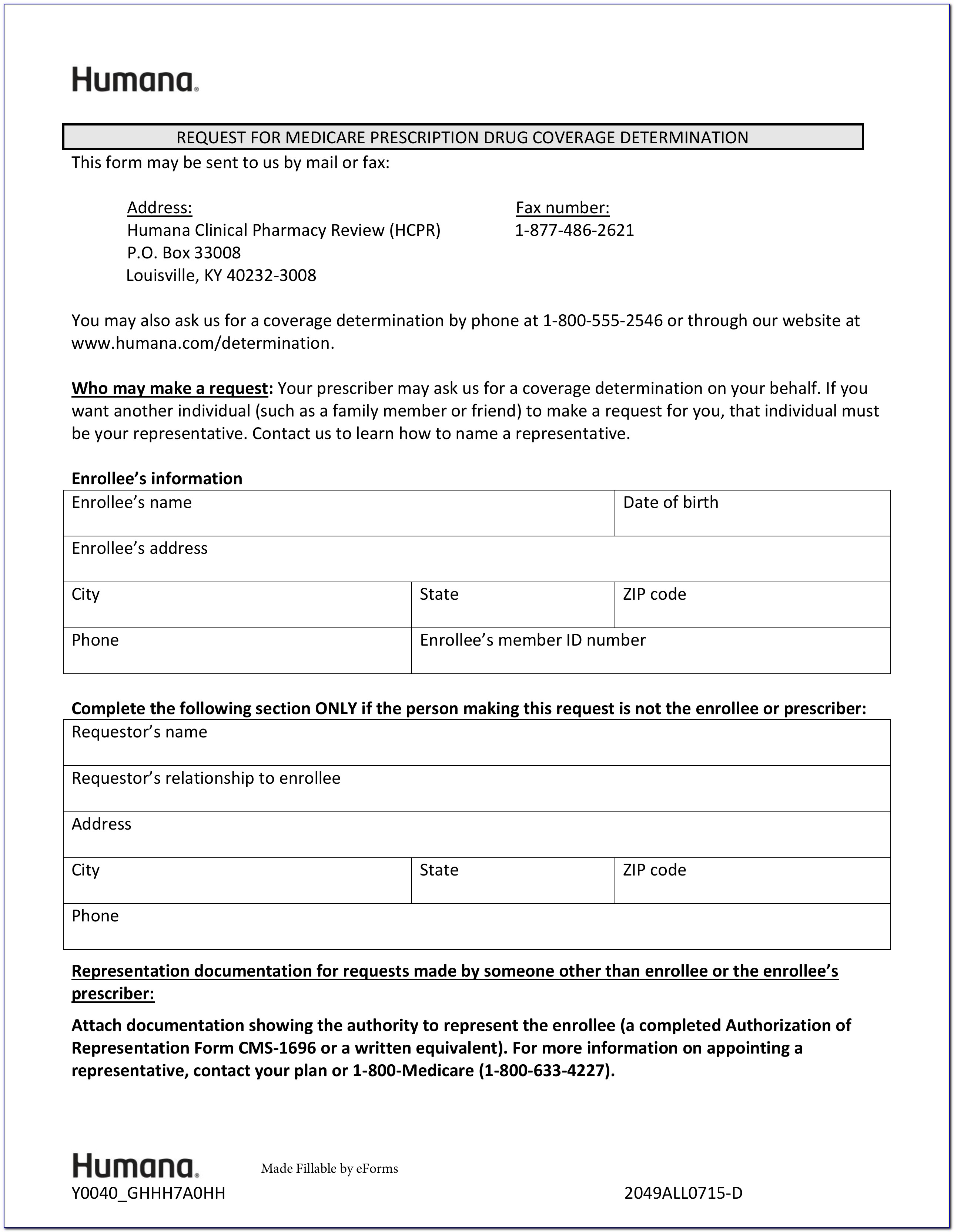
Aarp Medicare Part B Prior Authorization Form Form Resume Examples
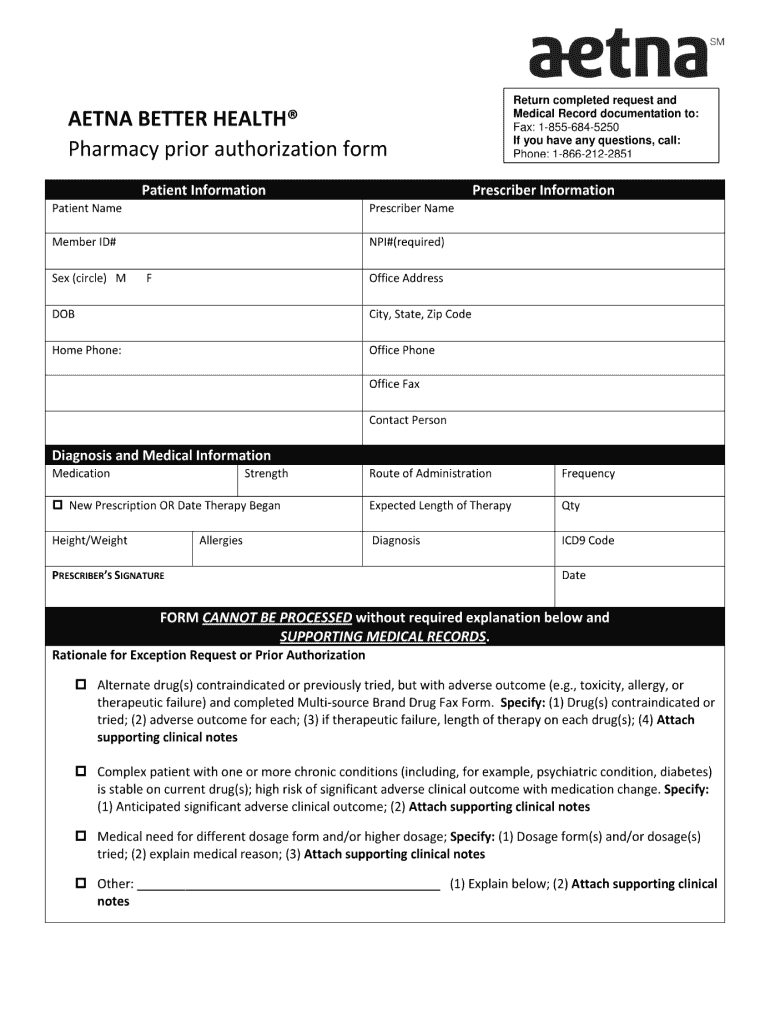
Web this patient’s benefit plan requires prior authorization for certain medications in order for the drug to be covered. Web precertification of belimumab (benlysta) is required of all aetna participating vendors and members in applicable design. Web precertification of belimumab (benlysta) is imperative of all health participating services and member in applicable plan. Web here’s how it works: Web benlysta.
Aetna Medicare Medication Prior Authorization Form Form Resume
Web o benlysta is initiated and titrated according to us food and drug administration labeled dosing for sle; Web updated june 02, 2022. Web prior authorization form all fields on this form are required. Web precertification of belimumab (benlysta) is required of all aetna participating providers and members in applicable plan designs. Submit your initial request on availity with the.
Covermymeds Humana Prior Auth Form Key.covermymeds Prior
We call this prior authorization. Web specialty medication precertification request please indicate: An aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not. Web belimumab (benlysta®) injectable medication precertification request (pdf, 366 kb) botulinum toxins medication. Please attach all clinical information.
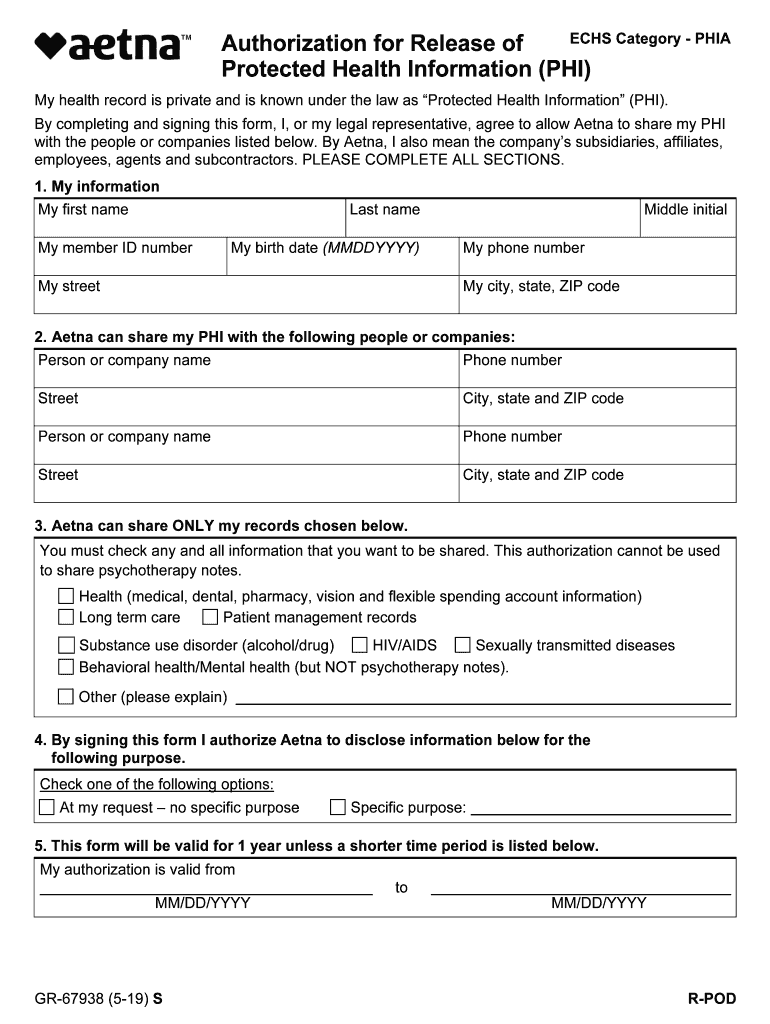
Aetna GR67938 S 20192021 Fill and Sign Printable Template Online
Some procedures, tests and prescriptions need prior approval to be sure they’re right for. Web pdf/ua accessible pdf aetna rx medical exceptio prior authrizatio precertifcation request for prescription medications. Web updated june 02, 2022. Please attach all clinical information. Submit your initial request on availity with the authorization (precertification) add transaction.
Aetna Medicare Prior Authorization Form Fill Online, Printable
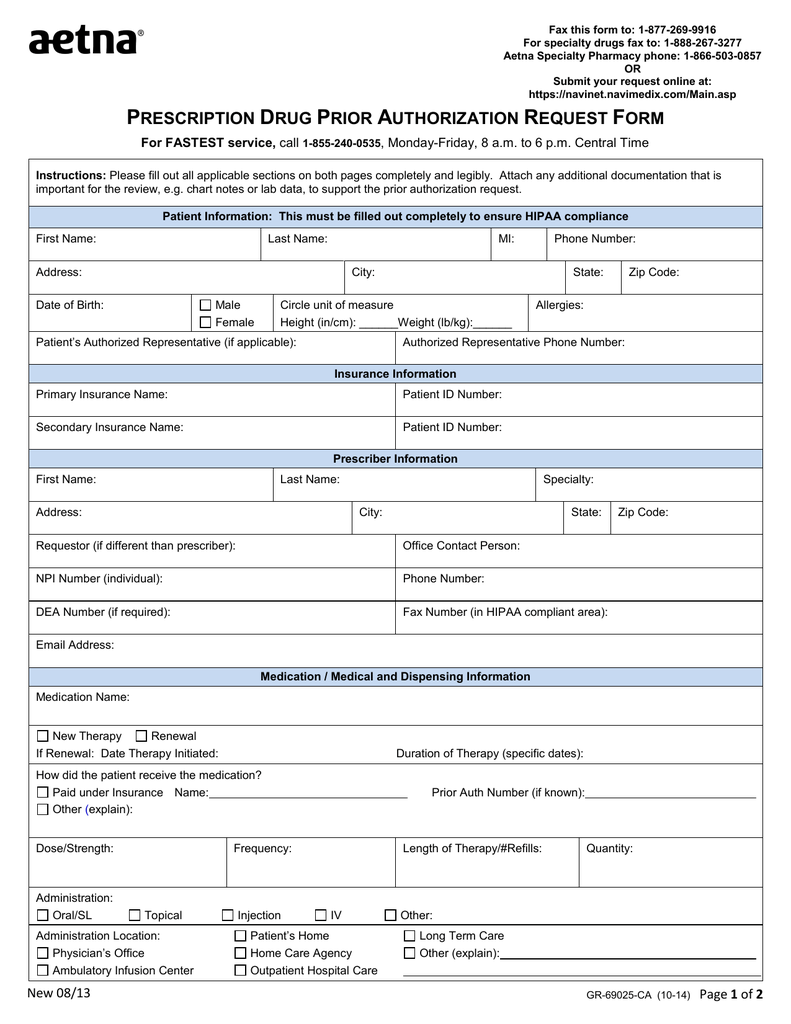
Web find all the forms you need. Check out how easy it is to complete and esign documents online. Web pdf/ua accessible pdf aetna rx medical exceptio prior authrizatio precertifcation request for prescription medications. Web precertification of belimumab (benlysta) is required of all aetna participating vendors and members in applicable design. Address, phone number and practice.
Aetna Prior Authorization Form Pdf Fill Out and Sign Printable PDF
Web belimumab (benlysta®) injectable medication precertification request (pdf, 366 kb) botulinum toxins medication. Web complete the attached prior authorization form. Address, phone number and practice. Web here’s how it works: For custodial requests, we need the actual date of admission and prior coverage payer information.
Aetna Specialty Pharmacy Prior Authorization Form PharmacyWalls
Web o benlysta is initiated and titrated according to us food and drug administration labeled dosing for sle; And o initial authorization is for no more than 12 months. Check out how easy it is to complete and esign documents online. Web specialty medication precertification request please indicate: For custodial requests, we need the actual date of admission and prior.
Aetna Specialty Pharmacy Prior Authorization Form PharmacyWalls
Web what is prior authorization? Address, phone number and practice. Specialty medication precertification request page. Find forms and applications for health care professionals and patients, all in one place. Web benlysta fax completed form to:
And o initial authorization is for no more than 12 months. Web belimumab (benlysta®) injectable medication precertification request (pdf, 366 kb) botulinum toxins medication. We know pa requests are complex. Some procedures, tests and prescriptions need prior approval to be sure they’re right for. Web here’s how it works: Web precertification of belimumab (benlysta) is required of all aetna participating providers and members in applicable plan designs. Web precertification of belimumab (benlysta) is imperative of all health participating services and member in applicable plan. Web find all the forms you need. We may need more details before we can approve some care options and products. Web benlysta fax completed form to: Please attach all clinical information. Web updated june 02, 2022. An aetna prior authorization form is designated for medical offices when a particular patient’s insurance is not. Specialty medication precertification request page. We call this prior authorization. Web get information about aetna’s precertification requirements, including precertification lists and criteria for. Web what is prior authorization? Web [document weight prior to therapy and weight after therapy with the date the weights were taken_____] yes or no if yes to question 1 and the request is for. To make an appropriate determination,. Web benlysta® (belimumab) injectable medication precertification request page 1 of 2 (all fields must be completed and.
Web Complete The Attached Prior Authorization Form.
Web [document weight prior to therapy and weight after therapy with the date the weights were taken_____] yes or no if yes to question 1 and the request is for. Web o benlysta is initiated and titrated according to us food and drug administration labeled dosing for sle; Web find all the forms you need. And o initial authorization is for no more than 12 months.
Web Benlysta Fax Completed Form To:
Address, phone number and practice. That's why we have a team of experts and a variety of help resources to. We know pa requests are complex. Web benlysta® (belimumab) injectable medication precertification request page 1 of 2 (all fields must be completed and.
To Make An Appropriate Determination,.
Check out how easy it is to complete and esign documents online. We may need more details before we can approve some care options and products. Please attach all clinical information. Web precertification of belimumab (benlysta) is required of all aetna participating vendors and members in applicable design.
An Aetna Prior Authorization Form Is Designated For Medical Offices When A Particular Patient’s Insurance Is Not.
Web what is prior authorization? Find forms and applications for health care professionals and patients, all in one place. Web view and download provider related prior authorization information at aetna better health of michigan. Web precertification of belimumab (benlysta) is required of all aetna participating providers and members in applicable plan designs.